| Fever | |
|---|---|
| Other names | Pyrexia, febrile response, febrile[1] |
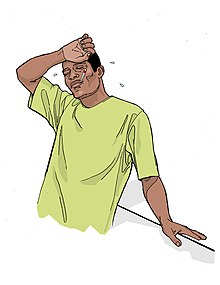 | |
| Person with fever | |
| Specialty | Infectious disease, pediatrics |
| Symptoms | Initially: shivering, feeling cold, chills[2] Later: flushed, sweating[3] |
| Complications | Febrile seizure[4] |
| Causes | Virus, bacteria, increase in the body's temperature set point[5][6] |
| Diagnostic method | Temperature higher than the normal range of 37.2 and 38.3 °C (99.0 and 100.9 °F)[1][7][8] |
| Differential diagnosis | Hyperthermia[1] |
| Treatment | Based on underlying cause, not required for fever itself[2][9] |
| Medication | Ibuprofen, paracetamol (acetaminophen)[9][10] |
| Frequency | Common[2][11] |
Fever or pyrexia in humans is a symptom of an anti-infection defense mechanism that appears with body temperature exceeding the normal range due to an increase in the body's temperature set point in the hypothalamus.[5][6][12][7] There is no single agreed-upon upper limit for normal temperature: sources use values ranging between 37.2 and 38.3 °C (99.0 and 100.9 °F) in humans.[1][7][8]
The increase in set point triggers increased muscle contractions and causes a feeling of cold or chills.[2] This results in greater heat production and efforts to conserve heat.[3] When the set point temperature returns to normal, a person feels hot, becomes flushed, and may begin to sweat.[3] Rarely a fever may trigger a febrile seizure, with this being more common in young children.[4] Fevers do not typically go higher than 41 to 42 °C (106 to 108 °F).[6]
A fever can be caused by many medical conditions ranging from non-serious to life-threatening.[13] This includes viral, bacterial, and parasitic infections—such as influenza, the common cold, meningitis, urinary tract infections, appendicitis, Lassa fever, COVID-19, and malaria.[13][14] Non-infectious causes include vasculitis, deep vein thrombosis, connective tissue disease, side effects of medication or vaccination, and cancer.[13][15] It differs from hyperthermia, in that hyperthermia is an increase in body temperature over the temperature set point, due to either too much heat production or not enough heat loss.[1]
Treatment to reduce fever is generally not required.[2][9] Treatment of associated pain and inflammation, however, may be useful and help a person rest.[9] Medications such as ibuprofen or paracetamol (acetaminophen) may help with this as well as lower temperature.[9][10] Children younger than three months require medical attention, as might people with serious medical problems such as a compromised immune system or people with other symptoms.[16] Hyperthermia requires treatment.[2]
Fever is one of the most common medical signs.[2] It is part of about 30% of healthcare visits by children[2] and occurs in up to 75% of adults who are seriously sick.[11] While fever evolved as a defense mechanism, treating a fever does not appear to improve or worsen outcomes.[17][18][19] Fever is often viewed with greater concern by parents and healthcare professionals than is usually deserved, a phenomenon known as "fever phobia."[2][20]
Associated symptoms
[edit]A fever is usually accompanied by sickness behavior, which consists of lethargy, depression, loss of appetite, sleepiness, hyperalgesia, dehydration,[21][22] and the inability to concentrate. Sleeping with a fever can often cause intense or confusing nightmares, commonly called "fever dreams".[23] Mild to severe delirium (which can also cause hallucinations) may also present itself during high fevers.[24]
Diagnosis
[edit]| Temperature classification | ||||||||||||
|
||||||||||||
| Note: The difference between fever and hyperthermia is the underlying mechanism. Different sources have different cut-offs for fever, hyperthermia and hyperpyrexia. | ||||||||||||
A range for normal temperatures has been found.[8] Central temperatures, such as rectal temperatures, are more accurate than peripheral temperatures.[30] Fever is generally agreed to be present if the elevated temperature[31] is caused by a raised set point and:
- Temperature in the anus (rectum/rectal) is at or over 37.5–38.3 °C (99.5–100.9 °F).[1][8] An ear (tympanic) or forehead (temporal) temperature may also be used.[32][33]
- Temperature in the mouth (oral) is at or over 37.2 °C (99.0 °F) in the morning or over 37.7 °C (99.9 °F) in the afternoon[7][34]
- Temperature under the arm (axillary) is usually about 0.6 °C (1.1 °F) below core body temperature.[35]
In adults, the normal range of oral temperatures in healthy individuals is 35.7–37.7 °C (96.3–99.9 °F) among men and 33.2–38.1 °C (91.8–100.6 °F) among women, while when taken rectally it is 36.7–37.5 °C (98.1–99.5 °F) among men and 36.8–37.1 °C (98.2–98.8 °F) among women, and for ear measurement it is 35.5–37.5 °C (95.9–99.5 °F) among men and 35.7–37.5 °C (96.3–99.5 °F) among women.[36]
Normal body temperatures vary depending on many factors, including age, sex, time of day, ambient temperature, activity level, and more.[37][38] Normal daily temperature variation has been described as 0.5 °C (0.9 °F).[7]: 4012 A raised temperature is not always a fever.[37] For example, the temperature rises in healthy people when they exercise, but this is not considered a fever, as the set point is normal.[37] On the other hand, a "normal" temperature may be a fever, if it is unusually high for that person; for example, medically frail elderly people have a decreased ability to generate body heat, so a "normal" temperature of 37.3 °C (99.1 °F) may represent a clinically significant fever.[37][39]
Hyperthermia
[edit]Hyperthermia is an elevation of body temperature over the temperature set point, due to either too much heat production or not enough heat loss.[1][7] Hyperthermia is thus not considered fever.[7]: 103 [40] Hyperthermia should not be confused with hyperpyrexia (which is a very high fever).[7]: 102
Clinically, it is important to distinguish between fever and hyperthermia as hyperthermia may quickly lead to death and does not respond to antipyretic medications. The distinction may however be difficult to make in an emergency setting, and is often established by identifying possible causes.[7]: 103
Types
[edit]
Various patterns of measured patient temperatures have been observed, some of which may be indicative of a particular medical diagnosis:
- Continuous fever, where temperature remains above normal and does not fluctuate more than 1 °C in 24 hours[41] (e.g. in bacterial pneumonia, typhoid fever, infective endocarditis, tuberculosis, or typhus).[42][43]
- Intermittent fever is present only for a certain period, later cycling back to normal (e.g., in malaria, leishmaniasis, pyemia, sepsis,[44] or African trypanosomiasis).[45]
- Remittent fever, where the temperature remains above normal throughout the day and fluctuates more than 1 °C in 24 hours (e.g., in infective endocarditis or brucellosis).[46]
- Pel–Ebstein fever is a cyclic fever that is rarely seen in patients with Hodgkin's lymphoma.
- Undulant fever, seen in brucellosis.
- Typhoid fever is a continuous fever showing a characteristic step-ladder pattern, a step-wise increase in temperature with a high plateau.[47]
Among the types of intermittent fever are ones specific to cases of malaria caused by different pathogens. These are:[48][49]
- Quotidian fever, with a 24-hour periodicity, typical of malaria caused by Plasmodium knowlesi (P. knowlesi);[50][51]
- Tertian fever, with a 48-hour periodicity, typical of later course malaria caused by P. falciparum, P. vivax, or P. ovale;[48]
- Quartan fever, with a 72-hour periodicity, typical of later course malaria caused by P. malariae.[48]
In addition, there is disagreement regarding whether a specific fever pattern is associated with Hodgkin's lymphoma—the Pel–Ebstein fever, with patients argued to present high temperature for one week, followed by low for the next week, and so on, where the generality of this pattern is debated.[52][53]
Persistent fever that cannot be explained after repeated routine clinical inquiries is called fever of unknown origin.[7][54] A neutropenic fever, also called febrile neutropenia, is a fever in the absence of normal immune system function.[55] Because of the lack of infection-fighting neutrophils, a bacterial infection can spread rapidly; this fever is, therefore, usually considered to require urgent medical attention.[56] This kind of fever is more commonly seen in people receiving immune-suppressing chemotherapy than in apparently healthy people.[55][57]
Hyperpyrexia
[edit]Hyperpyrexia is an extreme elevation of body temperature which, depending upon the source, is classified as a core body temperature greater than or equal to 40 or 41 °C (104 or 106 °F); the range of hyperpyrexia includes cases considered severe (≥ 40 °C) and extreme (≥ 42 °C).[7][58][59] It differs from hyperthermia in that one's thermoregulatory system's set point for body temperature is set above normal, then heat is generated to achieve it. In contrast, hyperthermia involves body temperature rising above its set point due to outside factors.[7][60] The high temperatures of hyperpyrexia are considered medical emergencies, as they may indicate a serious underlying condition or lead to severe morbidity (including permanent brain damage), or to death.[61] A common cause of hyperpyrexia is an intracranial hemorrhage.[7] Other causes in emergency room settings include sepsis, Kawasaki syndrome,[62] neuroleptic malignant syndrome, drug overdose, serotonin syndrome, and thyroid storm.[61]
Differential diagnosis
[edit]Fever is a common symptom of many medical conditions:
- Infectious disease, e.g., COVID-19,[14] dengue, Ebola, gastroenteritis, HIV, influenza, Lyme disease, rocky mountain spotted fever, secondary syphilis, malaria, mononucleosis, as well as infections of the skin, e.g., abscesses and boils.[63][64][65][66][67][68]
- Immunological diseases, e.g., relapsing polychondritis,[69] autoimmune hepatitis, granulomatosis with polyangiitis, Horton disease, inflammatory bowel diseases, Kawasaki disease, lupus erythematosus, sarcoidosis, Still's disease, rheumatoid arthritis, lymphoproliferative disorders and psoriasis;[citation needed]
- Tissue destruction, as a result of cerebral bleeding, crush syndrome, hemolysis, infarction, rhabdomyolysis, surgery, etc.;[70][71]
- Cancers, particularly blood cancers such as leukemia and lymphomas;[72]
- Metabolic disorders, e.g., gout, and porphyria;[73] and[74]
- Inherited metabolic disorder, e.g., Fabry disease.[7]
Adult and pediatric manifestations for the same disease may differ; for instance, in COVID-19, one metastudy describes 92.8% of adults versus 43.9% of children presenting with fever.[14]
In addition, fever can result from a reaction to an incompatible blood product.[75]
Function
[edit]
Hypothermia: Characterized in the center: Normal body temperature is shown in green, while the hypothermic temperature is shown in blue. As can be seen, hypothermia can be conceptualized as a decrease below the thermoregulatory set point.
Fever: Characterized on the right: Normal body temperature is shown in green. It reads "New Normal" because the thermoregulatory set point has risen. This has caused what was the normal body temperature (in blue) to be considered hypothermic.
Immune function
[edit]Fever is thought to contribute to host defense,[17] as the reproduction of pathogens with strict temperature requirements can be hindered, and the rates of some important immunological reactions are increased by temperature.[76] Fever has been described in teaching texts as assisting the healing process in various ways, including:
- increased mobility of leukocytes;[77]: 1044
- enhanced leukocyte phagocytosis;[77]: 1030
- decreased endotoxin effects;[77]: 1029 and
- increased proliferation of T cells.[77]: 1030 [78]: 212
Advantages and disadvantages
[edit]A fever response to an infectious disease is generally regarded as protective, whereas fever in non-infections may be maladaptive.[79][80] Studies have not been consistent on whether treating fever generally worsens or improves mortality risk.[81] Benefits or harms may depend on the type of infection, health status of the patient and other factors.[79] Studies using warm-blooded vertebrates suggest that they recover more rapidly from infections or critical illness due to fever.[82] In sepsis, fever is associated with reduced mortality.[83]
Pathophysiology of fever induction
[edit]Hypothalamus
[edit]Temperature is regulated in the hypothalamus. The trigger of a fever, called a pyrogen, results in the release of prostaglandin E2 (PGE2). PGE2 in turn acts on the hypothalamus, which creates a systemic response in the body, causing heat-generating effects to match a new higher temperature set point. There are four receptors in which PGE2 can bind (EP1-4), with a previous study showing the EP3 subtype is what mediates the fever response.[84] Hence, the hypothalamus can be seen as working like a thermostat.[7] When the set point is raised, the body increases its temperature through both active generation of heat and retention of heat. Peripheral vasoconstriction both reduces heat loss through the skin and causes the person to feel cold. Norepinephrine increases thermogenesis in brown adipose tissue, and muscle contraction through shivering raises the metabolic rate.[85]
If these measures are insufficient to make the blood temperature in the brain match the new set point in the hypothalamus, the brain orchestrates heat effector mechanisms via the autonomic nervous system or primary motor center for shivering. These may be:[86]
- Increased heat production by increased muscle tone, shivering (muscle movements to produce heat) and release of hormones like epinephrine; and
- Prevention of heat loss, e.g., through vasoconstriction.
When the hypothalamic set point moves back to baseline—either spontaneously or via medication—normal functions such as sweating, and the reverse of the foregoing processes (e.g., vasodilation, end of shivering, and nonshivering heat production) are used to cool the body to the new, lower setting.[citation needed]
This contrasts with hyperthermia, in which the normal setting remains, and the body overheats through undesirable retention of excess heat or over-production of heat. Hyperthermia is usually the result of an excessively hot environment (heat stroke) or an adverse reaction to drugs. Fever can be differentiated from hyperthermia by the circumstances surrounding it and its response to anti-pyretic medications.[7][verification needed]
In infants, the autonomic nervous system may also activate brown adipose tissue to produce heat (non-shivering thermogenesis).[87]
Increased heart rate and vasoconstriction contribute to increased blood pressure in fever.[88]
Pyrogens
[edit]A pyrogen is a substance that induces fever.[89] In the presence of an infectious agent, such as bacteria, viruses, viroids, etc., the immune response of the body is to inhibit their growth and eliminate them. The most common pyrogens are endotoxins, which are lipopolysaccharides (LPS) produced by Gram-negative bacteria such as E. coli. But pyrogens include non-endotoxic substances (derived from microorganisms other than gram-negative-bacteria or from chemical substances) as well.[90] The types of pyrogens include internal (endogenous) and external (exogenous) to the body.[91]
The "pyrogenicity" of given pyrogens varies: in extreme cases, bacterial pyrogens can act as superantigens and cause rapid and dangerous fevers.[92]
Endogenous
[edit]Endogenous pyrogens are cytokines released from monocytes (which are part of the immune system).[93] In general, they stimulate chemical responses, often in the presence of an antigen, leading to a fever. Whilst they can be a product of external factors like exogenous pyrogens, they can also be induced by internal factors like damage associated molecular patterns such as cases like rheumatoid arthritis or lupus.[94]
Major endogenous pyrogens are interleukin 1 (α and β)[95]: 1237–1248 and interleukin 6 (IL-6).[96] Minor endogenous pyrogens include interleukin-8, tumor necrosis factor-β, macrophage inflammatory protein-α and macrophage inflammatory protein-β as well as interferon-α, interferon-β, and interferon-γ.[95]: 1237–1248 Tumor necrosis factor-α (TNF) also acts as a pyrogen, mediated by interleukin 1 (IL-1) release.[97] These cytokine factors are released into general circulation, where they migrate to the brain's circumventricular organs where they are more easily absorbed than in areas protected by the blood–brain barrier.[98] The cytokines then bind to endothelial receptors on vessel walls to receptors on microglial cells, resulting in activation of the arachidonic acid pathway.[99]
Of these, IL-1β, TNF, and IL-6 are able to raise the temperature setpoint of an organism and cause fever. These proteins produce a cyclooxygenase which induces the hypothalamic production of PGE2 which then stimulates the release of neurotransmitters such as cyclic adenosine monophosphate and increases body temperature.[100]
Exogenous
[edit]Exogenous pyrogens are external to the body and are of microbial origin. In general, these pyrogens, including bacterial cell wall products, may act on Toll-like receptors in the hypothalamus and elevate the thermoregulatory setpoint.[101]
An example of a class of exogenous pyrogens are bacterial lipopolysaccharides (LPS) present in the cell wall of gram-negative bacteria. According to one mechanism of pyrogen action, an immune system protein, lipopolysaccharide-binding protein (LBP), binds to LPS, and the LBP–LPS complex then binds to a CD14 receptor on a macrophage. The LBP-LPS binding to CD14 results in cellular synthesis and release of various endogenous cytokines, e.g., interleukin 1 (IL-1), interleukin 6 (IL-6), and tumor necrosis factor-alpha (TNFα). A further downstream event is activation of the arachidonic acid pathway.[102]
PGE2 release
[edit]PGE2 release comes from the arachidonic acid pathway. This pathway (as it relates to fever), is mediated by the enzymes phospholipase A2 (PLA2), cyclooxygenase-2 (COX-2), and prostaglandin E2 synthase. These enzymes ultimately mediate the synthesis and release of PGE2.[citation needed]
PGE2 is the ultimate mediator of the febrile response. The setpoint temperature of the body will remain elevated until PGE2 is no longer present. PGE2 acts on neurons in the preoptic area (POA) through the prostaglandin E receptor 3 (EP3). EP3-expressing neurons in the POA innervate the dorsomedial hypothalamus (DMH), the rostral raphe pallidus nucleus in the medulla oblongata (rRPa), and the paraventricular nucleus (PVN) of the hypothalamus. Fever signals sent to the DMH and rRPa lead to stimulation of the sympathetic output system, which evokes non-shivering thermogenesis to produce body heat and skin vasoconstriction to decrease heat loss from the body surface. It is presumed that the innervation from the POA to the PVN mediates the neuroendocrine effects of fever through the pathway involving pituitary gland and various endocrine organs.[citation needed]
Management
[edit]Fever does not necessarily need to be treated,[103] and most people with a fever recover without specific medical attention.[104] Although it is unpleasant, fever rarely rises to a dangerous level even if untreated.[105] Damage to the brain generally does not occur until temperatures reach 42.0 °C (107.6 °F), and it is rare for an untreated fever to exceed 40.6 °C (105.1 °F).[106] Treating fever in people with sepsis does not affect outcomes.[107] Small trials have shown no benefit of treating fevers of 38.5 °C (101.3 °F) or higher of critically ill patients in ICUs, and one trial was terminated early because patients receiving aggressive fever treatment were dying more often.[19]
According to the NIH, the two assumptions which are generally used to argue in favor of treating fevers have not been experimentally validated. These are that (1) a fever is noxious, and (2) suppression of a fever will reduce its noxious effect. Most of the other studies supporting the association of fever with poorer outcomes have been observational in nature. In theory, these critically ill patients and those faced with additional physiologic stress may benefit from fever reduction, but the evidence on both sides of the argument appears to be mostly equivocal.[19]
Conservative measures
[edit]Limited evidence supports sponging or bathing feverish children with tepid water.[108] The use of a fan or air conditioning may somewhat reduce the temperature and increase comfort. If the temperature reaches the extremely high level of hyperpyrexia, aggressive cooling is required (generally produced mechanically via conduction by applying numerous ice packs across most of the body or direct submersion in ice water).[61] In general, people are advised to keep adequately hydrated.[109] Whether increased fluid intake improves symptoms or shortens respiratory illnesses such as the common cold is not known.[110]
Medications
[edit]Medications that lower fevers are called antipyretics.[111] The antipyretic ibuprofen is effective in reducing fevers in children.[112] It is more effective than acetaminophen (paracetamol) in children.[112] Ibuprofen and acetaminophen may be safely used together in children with fevers.[113][114] The efficacy of acetaminophen by itself in children with fevers has been questioned.[115] Ibuprofen is also superior to aspirin in children with fevers.[116] Additionally, aspirin is not recommended in children and young adults (those under the age of 16 or 19 depending on the country) due to the risk of Reye's syndrome.[117]
Using both paracetamol and ibuprofen at the same time or alternating between the two is more effective at decreasing fever than using only paracetamol or ibuprofen.[118] It is not clear if it increases child comfort.[118] Response or nonresponse to medications does not predict whether or not a child has a serious illness.[119]
With respect to the effect of antipyretics on the risk of death in those with infection, studies have found mixed results, as of 2019.[120]
Epidemiology
[edit]Fever is one of the most common medical signs.[2] It is part of about 30% of healthcare visits by children,[2] and occurs in up to 75% of adults who are seriously sick.[11] About 5% of people who go to an emergency room have a fever.[121]
History
[edit]A number of types of fever were known as early as 460 BC to 370 BC when Hippocrates was practicing medicine including that due to malaria (tertian or every 2 days and quartan or every 3 days).[122] It also became clear around this time that fever was a symptom of disease rather than a disease in and of itself.[122]
Infections presenting with fever were a major source of mortality in humans for about 200,000 years. Until the late nineteenth century, approximately half of all humans died from infections before the age of fifteen.[123]
An older term, febricula (a diminutive form of the Latin word for fever), was once used to refer to a low-grade fever lasting only a few days. This term fell out of use in the early 20th century, and the symptoms it referred to are now thought to have been caused mainly by various minor viral respiratory infections.[124]
Society and culture
[edit]Mythology
[edit]
- Febris (fever in Latin) is the goddess of fever in Roman mythology. People with fevers would visit her temples.
- Tertiana and Quartana are the goddesses of tertian and quartan fevers of malaria in Roman mythology.[125]
- Jvarasura (fever-demon in Hindi) is the personification of fever and disease in Hindu and Buddhist mythology.
Pediatrics
[edit]Fever is often viewed with greater concern by parents and healthcare professionals than might be deserved, a phenomenon known as fever phobia,[2][126] which is based in both caregiver's and parents' misconceptions about fever in children. Among them, many parents incorrectly believe that fever is a disease rather than a medical sign, that even low fevers are harmful, and that any temperature even briefly or slightly above the oversimplified "normal" number marked on a thermometer is a clinically significant fever.[126] They are also afraid of harmless side effects like febrile seizures and dramatically overestimate the likelihood of permanent damage from typical fevers.[126] The underlying problem, according to professor of pediatrics Barton D. Schmitt, is that "as parents we tend to suspect that our children's brains may melt."[127] As a result of these misconceptions parents are anxious, give the child fever-reducing medicine when the temperature is technically normal or only slightly elevated, and interfere with the child's sleep to give the child more medicine.[126]
Other species
[edit]Fever is an important metric for the diagnosis of disease in domestic animals. The body temperature of animals, which is taken rectally, is different from one species to another. For example, a horse is said to have a fever above 101 °F (38.3 °C).[128] In species that allow the body to have a wide range of "normal" temperatures, such as camels,[129] whose body temperature varies as the environmental temperature varies,[130] the body temperature which constitutes a febrile state differs depending on the environmental temperature.[131] Fever can also be behaviorally induced by invertebrates that do not have immune-system based fever. For instance, some species of grasshopper will thermoregulate to achieve body temperatures that are 2–5 °C higher than normal in order to inhibit the growth of fungal pathogens such as Beauveria bassiana and Metarhizium acridum.[132] Honeybee colonies are also able to induce a fever in response to a fungal parasite Ascosphaera apis.[132]
References
[edit]- ^ a b c d e f g h i Axelrod YK, Diringer MN (May 2008). "Temperature management in acute neurologic disorders". Neurologic Clinics. 26 (2): 585–603, xi. doi:10.1016/j.ncl.2008.02.005. PMID 18514828.
- ^ a b c d e f g h i j k l Sullivan JE, Farrar HC (March 2011). "Fever and antipyretic use in children". Pediatrics. 127 (3): 580–587. doi:10.1542/peds.2010-3852. PMID 21357332.
- ^ a b c Huether, Sue E. (2014). Pathophysiology: The Biologic Basis for Disease in Adults and Children (7th ed.). Elsevier Health Sciences. p. 498. ISBN 978-0323293754.
- ^ a b CDC Staff (31 March 2020). "Taking Care of Someone Who is Sick: Caring for Someone Sick at Home". Archived from the original on 24 March 2015. Retrieved 8 May 2015.
- ^ a b Kluger MJ (2015). Fever: Its Biology, Evolution, and Function. Princeton University Press. p. 57. ISBN 978-1400869831.
- ^ a b c Garmel GM, Mahadevan SV, eds. (2012). "Fever in adults". An introduction to clinical emergency medicine (2nd ed.). Cambridge: Cambridge University Press. p. 375. ISBN 978-0521747769.
- ^ a b c d e f g h i j k l m n o p Dinarello CA, Porat R (2018). "Chapter 15: Fever". In Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo, J (eds.). Harrison's Principles of Internal Medicine. Vol. 1–2 (20th ed.). New York: McGraw-Hill. ISBN 9781259644030. Retrieved 31 March 2020.
- ^ a b c d e f Laupland KB (July 2009). "Fever in the critically ill medical patient". Critical Care Medicine. 37 (7 Suppl): S273-8. doi:10.1097/CCM.0b013e3181aa6117. PMID 19535958.
- ^ a b c d e Richardson M, Purssell E (September 2015). "Who's afraid of fever?". Archives of Disease in Childhood. 100 (9): 818–820. doi:10.1136/archdischild-2014-307483. PMID 25977564. S2CID 206857750.
- ^ a b Garmel GM, Mahadevan SV, eds. (2012). An introduction to clinical emergency medicine (2nd ed.). Cambridge: Cambridge University Press. p. 401. ISBN 978-0521747769.
- ^ a b c Kiekkas P, Aretha D, Bakalis N, Karpouhtsi I, Marneras C, Baltopoulos GI (August 2013). "Fever effects and treatment in critical care: literature review". Australian Critical Care. 26 (3): 130–135. doi:10.1016/j.aucc.2012.10.004. PMID 23199670.
- ^ Franjić, Siniša (31 March 2019). "Fever Can Be A Symptom of Many Diseases". Journal of Medicine and HealthCare: 1–3. doi:10.47363/jmhc/2021(3)146. S2CID 243837498.
- ^ a b c Garmel GM, Mahadevan SV, eds. (2012). An introduction to clinical emergency medicine (2nd ed.). Cambridge: Cambridge University Press. p. 5. ISBN 978-0521747769.
- ^ a b c Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, Alvarado-Arnez LE, Bonilla-Aldana DK, Franco-Paredes C (13 March 2020). "Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis". Travel Medicine and Infectious Disease. 34: 101623. doi:10.1016/j.tmaid.2020.101623. PMC 7102608. PMID 32179124.
- ^ Dayal R, Agarwal D (January 2016). "Fever in Children and Fever of Unknown Origin". Indian Journal of Pediatrics. 83 (1): 38–43. doi:10.1007/s12098-015-1724-4. PMID 25724501. S2CID 34481402.
- ^ "Fever". MedlinePlus. 30 August 2014. Archived from the original on 11 May 2009.
- ^ a b Schaffner A (March 2006). "Fieber – nützliches oder schädliches, zu behandelndes Symptom?" [Fever–useful or noxious symptom that should be treated?]. Therapeutische Umschau (in German). 63 (3): 185–188. doi:10.1024/0040-5930.63.3.185. PMID 16613288. Abstract alone is in German and in English.
- ^ Niven DJ, Stelfox HT, Laupland KB (June 2013). "Antipyretic therapy in febrile critically ill adults: A systematic review and meta-analysis". Journal of Critical Care. 28 (3): 303–310. doi:10.1016/j.jcrc.2012.09.009. PMID 23159136.
- ^ a b c Ray, Juliet J. (December 2015). "Fever: suppress or let it ride?". Journal of Thoracic Disease. 7 (12): E633–E636. doi:10.3978/j.issn.2072-1439.2015.12.28. PMC 4703655. PMID 26793378.
- ^ Crocetti M, Moghbeli N, Serwint J (June 2001). "Fever Phobia Revisited: Have Parental Misconceptions About Fever Changed in 20 Years?". Pediatrics. 107 (6): 1241–1246. doi:10.1542/peds.107.6.1241. PMID 11389237.
- ^ "Fever: Symptoms, treatments, types, and causes". www.medicalnewstoday.com. 5 May 2020. Retrieved 22 April 2022.
- ^ Harden, L. M.; Kent, S.; Pittman, Q. J.; Roth, J. (1 November 2015). "Fever and sickness behavior: Friend or foe?". Brain, Behavior, and Immunity. 50: 322–333. doi:10.1016/j.bbi.2015.07.012. ISSN 0889-1591. PMID 26187566. S2CID 19396134.
- ^ Kelley KW, Bluthé RM, Dantzer R, Zhou JH, Shen WH, Johnson RW, Broussard SR (February 2003). "Cytokine-induced sickness behavior". Brain, Behavior, and Immunity. 17 Suppl 1 (1): S112–S118. doi:10.1016/S0889-1591(02)00077-6. PMID 12615196. S2CID 25400611.
- ^ Adamis D, Treloar A, Martin FC, Macdonald AJ (December 2007). "A brief review of the history of delirium as a mental disorder". History of Psychiatry. 18 (72 Pt 4): 459–469. doi:10.1177/0957154X07076467. PMID 18590023. S2CID 24424207.
- ^ Marx J (2006). Rosen's emergency medicine : concepts and clinical practice (6th ed.). Philadelphia: Mosby/Elsevier. p. 2239. ISBN 978-0-323-02845-5. OCLC 58533794.
- ^ Hutchison JS, Ward RE, Lacroix J, Hébert PC, Barnes MA, Bohn DJ, et al. (June 2008). "Hypothermia therapy after traumatic brain injury in children". The New England Journal of Medicine. 358 (23): 2447–56. doi:10.1056/NEJMoa0706930. PMID 18525042.
- ^ Pryor JA, Prasad AS (2008). Physiotherapy for Respiratory and Cardiac Problems: Adults and Paediatrics. Elsevier Health Sciences. p. 8. ISBN 978-0702039744.
Body temperature is maintained within the range 36.5-37.5 °C. It is lowest in the early morning and highest in the afternoon.
- ^ Grunau BE, Wiens MO, Brubacher JR (September 2010). "Dantrolene in the treatment of MDMA-related hyperpyrexia: a systematic review". Cjem. 12 (5): 435–42. doi:10.1017/s1481803500012598. PMID 20880437.
Dantrolene may also be associated with improved survival and reduced complications, especially in patients with extreme (≥ 42 °C) or severe (≥ 40 °C) hyperpyrexia
- ^ Sharma HS, ed. (2007). Neurobiology of Hyperthermia (1st ed.). Elsevier. pp. 175–177, 485. ISBN 9780080549996. Retrieved 19 November 2016.
Despite the myriad of complications associated with heat illness, an elevation of core temperature above 41.0 °C (often referred to as fever or hyperpyrexia) is the most widely recognized symptom of this syndrome.
- ^ Niven DJ, Gaudet JE, Laupland KB, Mrklas KJ, Roberts DJ, Stelfox HT (November 2015). "Accuracy of peripheral thermometers for estimating temperature: a systematic review and meta-analysis". Annals of Internal Medicine. 163 (10): 768–777. doi:10.7326/M15-1150. PMID 26571241. S2CID 4004360.
- ^ "Fever - Symptoms and causes". Mayo Clinic. Retrieved 23 April 2022.
- ^ "Measuring a Baby's Temperature". www.hopkinsmedicine.org. Archived from the original on 3 November 2019. Retrieved 10 September 2019.
- ^ "Tips for taking your child's temperature". Mayo Clinic. Retrieved 10 September 2019.
- ^ Barone JE (August 2009). "Fever: Fact and fiction". The Journal of Trauma. 67 (2): 406–409. doi:10.1097/TA.0b013e3181a5f335. PMID 19667898.
- ^ Pecoraro, Valentina; Petri, Davide; Costantino, Giorgio; Squizzato, Alessandro; Moja, Lorenzo; Virgili, Gianni; Lucenteforte, Ersilia (25 November 2020). "The diagnostic accuracy of digital, infrared and mercury-in-glass thermometers in measuring body temperature: a systematic review and network meta-analysis". Internal and Emergency Medicine. 16 (4). Springer Science and Business Media LLC: 1071–1083. doi:10.1007/s11739-020-02556-0. ISSN 1828-0447. PMC 7686821. PMID 33237494.
- ^ Sund-Levander M, Forsberg C, Wahren LK (June 2002). "Normal oral, rectal, tympanic and axillary body temperature in adult men and women: a systematic literature review". Scandinavian Journal of Caring Sciences. 16 (2): 122–128. doi:10.1046/j.1471-6712.2002.00069.x. PMID 12000664.
- ^ a b c d Garami, András; Székely, Miklós (6 May 2014). "Body temperature". Temperature: Multidisciplinary Biomedical Journal. 1 (1): 28–29. doi:10.4161/temp.29060. ISSN 2332-8940. PMC 4972507. PMID 27583277.
- ^ "Body temperature: What is the new normal?". www.medicalnewstoday.com. 12 January 2020. Retrieved 7 April 2020.
- ^ Alsalamah, M; Alrehaili, B; Almoamary, A; Al-Juad, A; Badri, M; El-Metwally, A (July 2022). "The optimal oral body temperature cutoff and other factors predictive of sepsis diagnosis in elderly patients". Annals of Thoracic Medicine. 17 (3): 159–165. doi:10.4103/atm.atm_52_22. PMC 9374123. PMID 35968398.
- ^ Beard, Robin M.; Day, Michael W. (June 2008). "Fever and Hyperthermia". Nursing2022. 38 (6): 28–31. doi:10.1097/01.NURSE.0000320353.79079.a5. ISSN 0360-4039. PMID 18497656.
- ^ Ogoina D (August 2011). "Fever, fever patterns and diseases called 'fever' – a review". Journal of Infection and Public Health. 4 (3): 108–124. doi:10.1016/j.jiph.2011.05.002. PMID 21843857.
- ^ Typhoid fever may show a specific fever pattern, with a slow stepwise increase and a high plateau (drops due to fever-reducing drugs are excluded).[citation needed]
- ^ Dall, Lawrence; Stanford, James F. (1990). "Fever, Chills, and Night Sweats". In Walker, H. Kenneth; Hall, W. Dallas; Hurst, J. Willis (eds.). Clinical Methods: The History, Physical, and Laboratory Examinations (3rd ed.). Boston: Butterworths. ISBN 0-409-90077-X. PMID 21250166.
- ^ Inayatullah, Muhammad; Nasir, Shabbir Ahmed (2016). Bedside Techniques: Methods of Clinical Examination (4th ed.). Paramount Books (Pvt.) Limited. ISBN 978-969-494-920-8.[page needed]
- ^ "African Trypanosomiasis – Disease". CDC. 28 April 2020. Archived from the original on 18 July 2021. Retrieved 18 July 2021.
- ^ "Brucella/Brucellosis". The Lecturio Medical Concept Library. Retrieved 19 July 2021.
- ^ "Enteric Fever (Typhoid Fever)". The Lecturio Medical Concept Library. 27 August 2020. Retrieved 19 July 2021.
- ^ a b c Ferri FF (2009). "Chapter 332. Protozoal infections". Ferri's Color Atlas and Text of Clinical Medicine. Elsevier Health Sciences. pp. 1159ff. ISBN 9781416049197. Archived from the original on 3 June 2016. Retrieved 31 March 2020.
- ^ Muhammad I, Nasir, SA (2009). Bedside Techniques: Methods of Clinical Examination. Multan, Pakistan: Saira Publishers/Salamat Iqbal Press.[page needed][better source needed]
- ^ Singh, B.; Daneshvar, C. (1 April 2013). "Human Infections and Detection of Plasmodium knowlesi". Clinical Microbiology Reviews. 26 (2): 165–184. doi:10.1128/CMR.00079-12. PMC 3623376. PMID 23554413.
- ^ Chin, W.; Contacos, P. G.; Coatney, G. R.; Kimball, H. R. (20 August 1965). "A Naturally Acquired Quotidian-Type Malaria in Man Transferable to Monkeys". Science. 149 (3686): 865. Bibcode:1965Sci...149..865C. doi:10.1126/science.149.3686.865. PMID 14332847. S2CID 27841173.
- ^ "Hodgkin Lymphoma: Practice Essentials, Background, Pathophysiology". Medscape. 9 November 2021.
- ^ Hilson AJ (July 1995). "Pel-Ebstein fever". The New England Journal of Medicine. 333 (1): 66–67. doi:10.1056/NEJM199507063330118. PMID 7777006., which cites Richard Asher's lecture, "Making Sense" [Lancet (1959) 2: 359].
- ^ Magrath, Melissa; Pearlman, Michelle; Peng, Lan; Lee, William (30 June 2018). "Granulomatous Hepatitis and Persistent Fever of Unknown Origin: A Case Report". Gastroenterology, Hepatology & Digestive Disorders. 1 (2): 1–2. doi:10.33425/2639-9334.1009. ISSN 2639-9334. S2CID 86786427.
- ^ a b Klastersky, Jean A. (2014), "Prevention of Febrile Neutropenia", Febrile Neutropenia, Tarporley: Springer Healthcare Ltd., pp. 13–26, doi:10.1007/978-1-907673-70-2_2, ISBN 978-1-907673-69-6, retrieved 22 April 2022
- ^ White, Lindsey; Ybarra, Michael (1 December 2017). "Neutropenic Fever". Hematology/Oncology Clinics of North America. 31 (6): 981–993. doi:10.1016/j.hoc.2017.08.004. PMID 29078933 – via ClinicalKey.
- ^ Rolston, Kenneth VI; Rubenstein, Edward B., eds. (2001). Textbook of febrile neutropenia. Martin Dunitz. ISBN 978-1-84184-033-8. OCLC 48195937.
- ^ Grunau BE, Wiens MO, Brubacher JR (September 2010). "Dantrolene in the treatment of MDMA-related hyperpyrexia: a systematic review". Canadian Journal of Emergency Medicine. 12 (5): 435–442. doi:10.1017/s1481803500012598. PMID 20880437.
Dantrolene may also be associated with improved survival and reduced complications, especially in patients with extreme (≥ 42 °C) or severe (≥ 40 °C) hyperpyrexia
- ^ Sharma HS, ed. (2007). Neurobiology of Hyperthermia (1st ed.). Elsevier. pp. 175–177, 485. ISBN 978-0080549996. Archived from the original on 8 September 2017. Retrieved 19 November 2016.
Despite the myriad of complications associated with heat illness, an elevation of core temperature above 41.0 °C (often referred to as fever or hyperpyrexia) is the most widely recognized symptom of this syndrome.
- ^ See section in Chapter 15 therein, the section on "Fever versus hyperthermia".
- ^ a b c McGugan EA (March 2001). "Hyperpyrexia in the emergency department". Emergency Medicine. 13 (1): 116–120. doi:10.1046/j.1442-2026.2001.00189.x. PMID 11476402.
- ^ Marx (2006), p. 2506.
- ^ Raoult, Didier; Levy, Pierre-Yves; Dupont, Hervé Tissot; Chicheportiche, Colette; Tamalet, Catherine; Gastaut, Jean-Albert; Salducci, Jacques (January 1993). "Q fever and HIV infection". AIDS. 7 (1): 81–86. doi:10.1097/00002030-199301000-00012. ISSN 0269-9370. PMID 8442921.
- ^ French, Neil; Nakiyingi, Jessica; Lugada, Eric; Watera, Christine; Whitworth, James A. G.; Gilks, Charles F. (May 2001). "Increasing rates of malarial fever with deteriorating immune status in HIV-1-infected Ugandan adults". AIDS. 15 (7): 899–906. doi:10.1097/00002030-200105040-00010. ISSN 0269-9370. PMID 11399962. S2CID 25470703. Archived from the original on 22 February 2022.
- ^ Heymann, D. L.; Weisfeld, J. S.; Webb, P. A.; Johnson, K. M.; Cairns, T.; Berquist, H. (1 September 1980). "Ebola Hemorrhagic Fever: Tandala, Zaire, 1977–1978". Journal of Infectious Diseases. 142 (3): 372–376. doi:10.1093/infdis/142.3.372. ISSN 0022-1899. PMID 7441008.
- ^ Feldmann, Heinz; Geisbert, Thomas W (March 2011). "Ebola haemorrhagic fever". The Lancet. 377 (9768): 849–862. doi:10.1016/s0140-6736(10)60667-8. ISSN 0140-6736. PMC 3406178. PMID 21084112.
- ^ Oakley, Miranda S.; Gerald, Noel; McCutchan, Thomas F.; Aravind, L.; Kumar, Sanjai (October 2011). "Clinical and molecular aspects of malaria fever". Trends in Parasitology. 27 (10): 442–449. doi:10.1016/j.pt.2011.06.004. ISSN 1471-4922. PMID 21795115.
- ^ Colunga-Salas, Pablo; Sánchez-Montes, Sokani; Volkow, Patricia; Ruíz-Remigio, Adriana; Becker, Ingeborg (17 September 2020). "Lyme disease and relapsing fever in Mexico: An overview of human and wildlife infections". PLOS ONE. 15 (9): e0238496. Bibcode:2020PLoSO..1538496C. doi:10.1371/journal.pone.0238496. ISSN 1932-6203. PMC 7497999. PMID 32941463.
- ^ Puéchal X, Terrier B, Mouthon L, Costedoat-Chalumeau N, Guillevin L, Le Jeunne C (March 2014). "Relapsing polychondritis". Joint, Bone, Spine. 81 (2): 118–124. doi:10.1016/j.jbspin.2014.01.001. PMID 24556284. S2CID 205754989.
- ^ Arnhold, Jürgen (2020), "Cell and Tissue Destruction in Selected Disorders", Cell and Tissue Destruction, Elsevier, pp. 249–287, doi:10.1016/b978-0-12-816388-7.00009-7, ISBN 9780128163887, S2CID 209284148, retrieved 22 April 2022
- ^ Arnhold, Jürgen (2019). Cell and tissue destruction: mechanisms, protection, disorders. Elsevier Science. ISBN 978-0-12-816388-7. OCLC 1120070914.
- ^ "Signs and Symptoms of Cancer | Do I Have Cancer?". www.cancer.org. Retrieved 20 June 2020.
- ^ Centerwall, Willard R. (1965). Phenylketonuria: an inherited metabolic disorder associated with mental retardation. U.S. Department of Health, Education, and Welfare, Welfare Administration, Children's Bureau. OCLC 392284.
- ^ "Metabolic Disorder", Definitions, Qeios, 7 February 2020, doi:10.32388/7344b1, S2CID 42063856, retrieved 22 April 2022
- ^ Dean, Laura (2005). Blood transfusions and the immune system. National Center for Biotechnology Information (US).
- ^ Fischler MP, Reinhart WH (May 1997). "[Fever: friend or enemy?]". Schweizerische Medizinische Wochenschrift (in German). 127 (20): 864–870. PMID 9289813.
- ^ a b c d Craven RF, Hirnle CJ (2003). Fundamentals of Nursing: Human Health and Function (4th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. ISBN 9780781758185. Retrieved 2 April 2020.
- ^ Lewis SM, Dirksen SR, Heitkemper MM (2005). Medical-Surgical Nursing: Assessment and Management of Clinical Problems (6th ed.). Amsterdam, NL: Elsevier-Health Sciences. ISBN 9780323031059. Retrieved 2 April 2020.
- ^ a b Kiekkas P, Aretha D, Bakalis N, Karpouhtsi I, Marneras C, Baltopoulos GI (August 2013). "Fever effects and treatment in critical care: literature review". Australian Critical Care. 26 (3): 130–135. doi:10.1016/j.aucc.2012.10.004. PMID 23199670.
- ^ Kluger MJ, Kozak W, Conn CA, Leon LR, Soszynski D (September 1998). "Role of fever in disease". Annals of the New York Academy of Sciences. 856 (1): 224–233. Bibcode:1998NYASA.856..224K. doi:10.1111/j.1749-6632.1998.tb08329.x. PMID 9917881. S2CID 12408561.
- ^ Drewry, Anne M.; Ablordeppey, Enyo A.; Murray, Ellen T.; Stoll, Carolyn R. T.; Izadi, Sonya R.; Dalton, Catherine M.; Hardi, Angela C.; Fowler, Susan A.; Fuller, Brian M.; Colditz, Graham A. (2017). "Antipyretic Therapy in Critically Ill Septic Patients". Critical Care Medicine. 45 (5): 806–813. doi:10.1097/CCM.0000000000002285. PMC 5389594. PMID 28221185.
- ^ Su F, Nguyen ND, Wang Z, Cai Y, Rogiers P, Vincent JL (June 2005). "Fever control in septic shock: beneficial or harmful?". Shock. 23 (6): 516–520. PMID 15897803.
- ^ Rumbus, Z; Matics, R; Hegyi, P; et al. (2017). "Fever Is Associated with Reduced, Hypothermia with Increased Mortality in Septic Patients: A Meta-Analysis of Clinical Trials". PLOS ONE. 12 (1): e0170152. Bibcode:2017PLoSO..1270152R. doi:10.1371/journal.pone.0170152. PMC 5230786. PMID 28081244.
- ^ Ushikubi F, et al. (September 1998). "Impaired febrile response in mice lacking the prostaglandin E receptor subtype EP3". Nature. 395 (6699): 281–284. Bibcode:1998Natur.395..281U. doi:10.1038/26233. PMID 9751056. S2CID 4420632.
- ^ Evans SS, Repasky EA, Fisher DT (June 2015). "Fever and the thermal regulation of immunity: the immune system feels the heat". Nature Reviews. Immunology. 15 (6): 335–349. doi:10.1038/nri3843. PMC 4786079. PMID 25976513.
- ^ Tabarean, Iustin; Morrison, Brad; Marcondes, Maria Cecilia; Bartfai, Tamas; Conti, Bruno (January 2010). "Hypothalamic and dietary control of temperature-mediated longevity". Ageing Research Reviews. 9 (1): 41–50. doi:10.1016/j.arr.2009.07.004. ISSN 1872-9649. PMC 2818054. PMID 19631766.
- ^ Nowack, Julia; Giroud, Sylvain; Arnold, Walter; Ruf, Thomas (9 November 2017). "Muscle Non-shivering Thermogenesis and Its Role in the Evolution of Endothermy". Frontiers in Physiology. 8: 889. doi:10.3389/fphys.2017.00889. ISSN 1664-042X. PMC 5684175. PMID 29170642.
- ^ Deussen, A. (September 2007). "[Hyperthermia and hypothermia. Effects on the cardiovascular system]". Der Anaesthesist. 56 (9): 907–911. doi:10.1007/s00101-007-1219-4. ISSN 0003-2417. PMID 17554514.
- ^ Hagel L, Jagschies G, Sofer G (1 January 2008). "5 – Analysis". Handbook of Process Chromatography (2nd ed.). Academic Press. pp. 127–145. doi:10.1016/b978-012374023-6.50007-5. ISBN 978-0-12-374023-6.
- ^ Kojima K (1 January 2012). "17 – Biological evaluation and regulation of medical devices in Japan". In Boutrand JP (ed.). Biocompatibility and Performance of Medical Devices. Woodhead Publishing Series in Biomaterials. Woodhead Publishing. pp. 404–448. doi:10.1533/9780857096456.4.404. ISBN 978-0-85709-070-6. S2CID 107630997.
- ^ El-Radhi, A. Sahib (2018), El-Radhi, A. Sahib (ed.), "Pathogenesis of Fever", Clinical Manual of Fever in Children, Cham: Springer International Publishing: 53–68, doi:10.1007/978-3-319-92336-9_3, ISBN 978-3-319-92336-9, PMC 7122269, retrieved 26 June 2024
- ^ Affairs, Office of Regulatory (3 November 2018). "Pyrogens, Still a Danger". FDA.
- ^ Constable PD, Hinchcliff KW, Done SH, Grünberg W, eds. (1 January 2017). "4 – General Systemic States". Veterinary Medicine (11th ed.). W.B. Saunders. pp. 43–112. doi:10.1016/b978-0-7020-5246-0.00004-8. ISBN 978-0-7020-5246-0. S2CID 214758182.
- ^ Dinarello CA (31 March 2015). "The history of fever, leukocytic pyrogen and interleukin-1". Temperature. 2 (1): 8–16. doi:10.1080/23328940.2015.1017086. PMC 4843879. PMID 27226996.
- ^ a b Stitt, John (2008). "Chapter 59: Regulation of Body Temperature". In Boron WF, Boulpaep, EL (eds.). Medical Physiology: A Cellular and Molecular Approach (2nd ed.). Philadelphia: Elsevier Saunders. ISBN 9781416031154. Retrieved 2 April 2020.
- ^ Murphy, Kenneth (Kenneth M.) (2017). Janeway's immunobiology. Weaver, Casey (9th ed.). New York. pp. 118–119. ISBN 978-0-8153-4505-3. OCLC 933586700.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Stefferl A, Hopkins SJ, Rothwell NJ, Luheshi GN (August 1996). "The role of TNF-alpha in fever: opposing actions of human and murine TNF-alpha and interactions with IL-beta in the rat". British Journal of Pharmacology. 118 (8): 1919–1924. doi:10.1111/j.1476-5381.1996.tb15625.x. PMC 1909906. PMID 8864524.
- ^ Kennedy, Rachel H.; Silver, Rae (2016), Pfaff, Donald W.; Volkow, Nora D. (eds.), "Neuroimmune Signaling: Cytokines and the CNS", Neuroscience in the 21st Century, New York: Springer, pp. 1–41, doi:10.1007/978-1-4614-6434-1_174-1, ISBN 978-1-4614-6434-1, retrieved 26 June 2024
- ^ Eskilsson, Anna (2020). Inflammatory Signaling Across the Blood-Brain Barrier and the Generation of Fever. Linköping: Linköping University, Department of Biomedical and Clinical Sciences. ISBN 978-91-7929-936-1.
- ^ Srinivasan L, Harris MC, Kilpatrick LE (1 January 2017). "128 – Cytokines and Inflammatory Response in the Fetus and Neonate". In Polin RA, Abman SH, Rowitch DH, Benitz WE (eds.). Fetal and Neonatal Physiology (5th ed.). Elsevier. pp. 1241–1254.e4. doi:10.1016/b978-0-323-35214-7.00128-1. ISBN 978-0-323-35214-7.
- ^ Wilson ME, Boggild AK (1 January 2011). "130 – Fever and Systemic Symptoms". In Guerrant RL, Walker DH, Weller PF (eds.). Tropical Infectious Diseases: Principles, Pathogens and Practice (3rd ed.). W.B. Saunders. pp. 925–938. doi:10.1016/b978-0-7020-3935-5.00130-0. ISBN 978-0-7020-3935-5.
- ^ Roth J, Blatteis CM (October 2014). "Mechanisms of fever production and lysis: Lessons from experimental LPS fever". Comprehensive Physiology. 4 (4): 1563–1604. doi:10.1002/cphy.c130033. ISBN 9780470650714. PMID 25428854.
- ^ Ludwig J, McWhinnie H (May 2019). "Antipyretic drugs in patients with fever and infection: literature review". Br J Nurs. 28 (10): 610–618. doi:10.12968/bjon.2019.28.10.610. PMID 31116598. S2CID 162182092.
- ^ "What To Do If You Get Sick: 2009 H1N1 and Seasonal Flu". Centers for Disease Control and Prevention. 7 May 2009. Archived from the original on 3 November 2009. Retrieved 1 November 2009.
- ^ Klein, Natalie C.; Cunha, Burke A. (1 March 1996). "Treatment of Fever". Infectious Disease Clinics of North America. 10 (1): 211–216. doi:10.1016/S0891-5520(05)70295-6. ISSN 0891-5520. PMID 8698992.
- ^ Edward James Walter; Mike Carraretto (2016). "The neurological and cognitive consequences of hyperthermia". Critical Care. 20 (1): 199. doi:10.1186/s13054-016-1376-4. PMC 4944502. PMID 27411704.
- ^ Drewry AM, Ablordeppey EA, Murray ET, Stoll CR, Izadi SR, Dalton CM, Hardi AC, Fowler SA, Fuller BM, Colditz GA (May 2017). "Antipyretic Therapy in Critically Ill Septic Patients: A Systematic Review and Meta-Analysis". Critical Care Medicine. 45 (5): 806–813. doi:10.1097/CCM.0000000000002285. PMC 5389594. PMID 28221185.
- ^ Meremikwu M, Oyo-Ita A (2003). Meremikwu MM (ed.). "Physical methods for treating fever in children". The Cochrane Database of Systematic Reviews. 2003 (2): CD004264. doi:10.1002/14651858.CD004264. PMC 6532675. PMID 12804512.
- ^ "Fever". National Institute of Health. Archived from the original on 30 April 2016.
- ^ Guppy MP, Mickan SM, Del Mar CB, Thorning S, Rack A (February 2011). "Advising patients to increase fluid intake for treating acute respiratory infections". The Cochrane Database of Systematic Reviews. 2011 (2): CD004419. doi:10.1002/14651858.CD004419.pub3. PMC 7197045. PMID 21328268.
- ^ El-Radhi, A. S. (1 October 2000). "Physical treatment of fever". Archives of Disease in Childhood. 83 (4): 369c–369. doi:10.1136/adc.83.4.369c. ISSN 0003-9888. PMC 1718494. PMID 11032580.
- ^ a b Perrott DA, Piira T, Goodenough B, Champion GD (June 2004). "Efficacy and safety of acetaminophen vs ibuprofen for treating children's pain or fever: a meta-analysis". Archives of Pediatrics & Adolescent Medicine. 158 (6): 521–526. doi:10.1001/archpedi.158.6.521. PMID 15184213.
- ^ Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, Peters TJ (May 2009). "Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial". Health Technology Assessment. 13 (27): iii–iv, ix–x, 1–163. doi:10.3310/hta13270. hdl:10044/1/57595. PMID 19454182.
- ^ Southey ER, Soares-Weiser K, Kleijnen J (September 2009). "Systematic review and meta-analysis of the clinical safety and tolerability of ibuprofen compared with paracetamol in paediatric pain and fever". Current Medical Research and Opinion. 25 (9): 2207–2222. doi:10.1185/03007990903116255. PMID 19606950. S2CID 31653539.
- ^ Meremikwu M, Oyo-Ita A (2002). "Paracetamol for treating fever in children". The Cochrane Database of Systematic Reviews. 2002 (2): CD003676. doi:10.1002/14651858.CD003676. PMC 6532671. PMID 12076499.
- ^ Autret E, Reboul-Marty J, Henry-Launois B, Laborde C, Courcier S, Goehrs JM, Languillat G, Launois R (1997). "Evaluation of ibuprofen versus aspirin and paracetamol on efficacy and comfort in children with fever". European Journal of Clinical Pharmacology. 51 (5): 367–371. doi:10.1007/s002280050215. PMID 9049576. S2CID 27519225.
- ^ "2.9 Antiplatelet drugs". British National Formulary for Children. British Medical Association and Royal Pharmaceutical Society of Great Britain. 2007. p. 151.
- ^ a b Wong T, Stang AS, Ganshorn H, Hartling L, Maconochie IK, Thomsen AM, Johnson DW (October 2013). "Combined and alternating paracetamol and ibuprofen therapy for febrile children". The Cochrane Database of Systematic Reviews. 2013 (10): CD009572. doi:10.1002/14651858.CD009572.pub2. PMC 6532735. PMID 24174375.
- ^ King D (August 2013). "Question 2: does a failure to respond to antipyretics predict serious illness in children with a fever?". Archives of Disease in Childhood. 98 (8): 644–646. doi:10.1136/archdischild-2013-304497. PMID 23846358. S2CID 32438262.
- ^ Ludwig J, McWhinnie H (May 2019). "Antipyretic drugs in patients with fever and infection: literature review". British Journal of Nursing. 28 (10): 610–618. doi:10.12968/bjon.2019.28.10.610. PMID 31116598. S2CID 162182092.
- ^ Nassisi D, Oishi ML (January 2012). "Evidence-based guidelines for evaluation and antimicrobial therapy for common emergency department infections". Emergency Medicine Practice. 14 (1): 1–28, quiz 28–29. PMID 22292348.
- ^ a b Sajadi MM, Bonabi R, Sajadi MR, Mackowiak PA (October 2012). "Akhawayni and the first fever curve". Clinical Infectious Diseases. 55 (7): 976–980. doi:10.1093/cid/cis596. PMID 22820543.
- ^ Casanova, Jean-Laurent; Abel, Laurent (2021). "Lethal Infectious Diseases as Inborn Errors of Immunity: Toward a Synthesis of the Germ and Genetic Theories". Annual Review of Pathology: Mechanisms of Disease. 16: 23–50. doi:10.1146/annurev-pathol-031920-101429. PMC 7923385. PMID 32289233.
- ^ Straus, Bernard (September 1970) [first presented at a conference on 27 May 1970]. "Defunct and Dying Diseases". Bulletin of the New York Academy of Medicine. 46 (9): 686–706. PMC 1749762. PMID 4916301.
- ^ Scheid, John (22 December 2015), "Febris", Oxford Research Encyclopedia of Classics, Oxford University Press, doi:10.1093/acrefore/9780199381135.013.2651, ISBN 978-0-19-938113-5, retrieved 23 January 2023
- ^ a b c d Crocetti M, Moghbeli N, Serwint J (June 2001). "Fever Phobia Revisited: Have Parental Misconceptions About Fever Changed in 20 Years?". Pediatrics. 107 (6): 1241–1246. doi:10.1542/peds.107.6.1241. PMID 11389237. Retrieved 31 March 2020.
- ^ Klass, Perri (10 January 2011). "Lifting a Veil of Fear to See a Few Benefits of Fever". The New York Times. Archived from the original on 29 September 2015.
- ^ "Equusite Vital Signs". equusite.com. Archived from the original on 26 March 2010. Retrieved 22 March 2010.
- ^ Schmidt-Nielsen K, Schmidt-Nielsen B, Jarnum SA, Houpt TR (January 1957). "Body temperature of the camel and its relation to water economy". The American Journal of Physiology. 188 (1): 103–112. doi:10.1152/ajplegacy.1956.188.1.103. PMID 13402948.
- ^ Leese A (March 1917). "'Tips' on camels, for veterinary surgeons on active service". The British Veterinary Journal. 73: 81 – via Google Books.
- ^ Tefera M (July 2004). "Observations on the clinical examination of the camel (Camelus dromedarius) in the field". Tropical Animal Health and Production. 36 (5): 435–449. doi:10.1023/b:trop.0000035006.37928.cf. PMID 15449833. S2CID 26358556.
- ^ a b Thomas MB, Blanford S (July 2003). "Thermal biology in insect-parasite interactions". Trends in Ecology & Evolution. 18 (7): 344–350. doi:10.1016/S0169-5347(03)00069-7.
Further reading
[edit]- Rhoades R, Pflanzer RG (1996). "Chapter 27: Regulation of Body Temperature (Clinical Focus: Pathogenesis of Fever)". Human Physiology (3rd ed.). Philadelphia: Saunders College. ISBN 9780030051593. Retrieved 2 April 2020.
External links
[edit]- Fever and Taking Your Child's Temperature
- US National Institute of Health factsheet
- Drugs most commonly associated with the adverse event Pyrexia (Fever) as reported the FDA Archived 9 March 2012 at the Wayback Machine
- Fever at MedlinePlus
- Why are We So Afraid of Fevers? at The New York Times