| Arthritis | |
|---|---|
 | |
| A hand affected by rheumatoid arthritis, an autoimmune form of arthritis | |
| Pronunciation | |
| Specialty | Rheumatology |
| Symptoms | Joint pain, stiffness, redness, swelling, decreased range of motion[2][3] |
| Complications | Amplified musculoskeletal pain syndrome[4] |
| Types | > 100, most common (osteoarthritis, rheumatoid arthritis)[5][6][7] |
| Risk factors | Family history, age, sex trait, previous joint injury, obesity.[8] |
| Treatment | Resting, applying ice or heat, weight loss, exercise, joint replacement[7] |
| Medication | Ibuprofen, paracetamol (acetaminophen)[9] |
Arthritis is a general medical term used to describe a disorder that affects joints.[2] Symptoms generally include joint pain and stiffness.[2] Other symptoms may include redness, warmth, swelling, and decreased range of motion of the affected joints.[2][3] In certain types of arthritis, other organs such as the skin are also affected.[7] Onset can be gradual or sudden.[6]
There are several types of arthritis.[10][5][6] The most common forms are osteoarthritis (most commonly seen in weightbearing joints) and rheumatoid arthritis.[7] Osteoarthritis usually occurs as an individual ages and often affects the hips, knees, shoulders, and fingers.[7][11] Rheumatoid arthritis is an autoimmune disorder that often affects the hands and feet.[7] Other types of arthritis include gout, lupus, and septic arthritis.[7][12] These are inflammatory based types of rheumatic disease.[2]
Early treatment for arthritis commonly includes resting the affected joint and conservative measures such as heating or icing.[7][13] Weight loss and exercise may also be useful to reduce the force across a weightbearing joint.[7][14] Medication intervention for symptoms depends on the form of arthritis.[15][9] These may include anti-inflammatory medications such as ibuprofen and paracetamol (acetaminophen).[9] With severe cases of arthritis, joint replacement surgery may be necessary.[7]
Osteoarthritis is the most common form of arthritis affecting more than 3.8% of people, while rheumatoid arthritis is the second most common affecting about 0.24% of people.[16] In Australia about 15% of people are affected by arthritis,[17] while in the United States more than 20% have a type of arthritis.[12][18] Overall arthritis becomes more common with age.[12] Arthritis is a common reason people are unable to carryout their work and can result in decreased ability to complete activities of daily living.[9] The term arthritis is derived from arthr- (meaning 'joint') and -itis (meaning 'inflammation').[19][20]
Classification
[edit]There are several diseases where joint pain is the most prominent symptom. Generally when a person has "arthritis" it means that they have one of the following diseases:
- Hemarthrosis
- Osteoarthritis[21]
- Rheumatoid arthritis[22]
- Gout and pseudo-gout[23]
- Septic arthritis[24]
- Ankylosing spondylitis[25]
- Juvenile idiopathic arthritis[26]
- Still's disease[27]
- Psoriatic arthritis[28]
Joint pain can also be a symptom of other diseases. In this case, the person may not have arthritis and instead have one of the following diseases:
- Psoriasis[29]
- Reactive arthritis[30]
- Ehlers–Danlos syndrome[31]
- Iron overload[32]
- Hepatitis[33][34]
- Lyme disease[35]
- Sjögren's disease[36]
- Hashimoto's thyroiditis[37]
- Celiac disease[38]
- Non-celiac gluten sensitivity[39][40][41]
- Inflammatory bowel disease (including Crohn's disease and ulcerative colitis)[42][43]
- Henoch–Schönlein purpura[44]
- Hyperimmunoglobulinemia D with recurrent fever
- Sarcoidosis[45]
- Whipple's disease[46]
- TNF receptor associated periodic syndrome[47]
- Granulomatosis with polyangiitis (and many other vasculitis syndromes)
- Familial Mediterranean fever[48]
- Systemic lupus erythematosus[49]
An undifferentiated arthritis is an arthritis that does not fit into well-known clinical disease categories, possibly being an early stage of a definite rheumatic disease.[50]
Signs and symptoms
[edit]| Extra-articular features of joint disease[51] |
|---|
| Cutaneous nodules |
| Cutaneous vasculitis lesions |
| Lymphadenopathy |
| Oedema |
| Ocular inflammation |
| Urethritis |
| Tenosynovitis (tendon sheath effusions) |
| Bursitis (swollen bursa) |
| Diarrhea |
| Orogenital ulceration |
Pain in varying severity is a common symptom in most types of arthritis.[52][53] Other symptoms include swelling, joint stiffness, redness, and aching around the joint(s).[2] Arthritic disorders like lupus and rheumatoid arthritis can affect other organs in the body, leading to a variety of symptoms including:[12][2]
- Inability to use the hand or walk
- Stiffness in one or more joints
- Rash or itch
- Malaise and fatigue
- Weight loss
- Poor sleep
- Muscle aches and pains
- Tenderness
- Difficulty moving the joint
Causes
[edit]Some common risk factors that can increase the chances of developing osteoarthritis include obesity, prior injury to the joint, type of joint, and muscle strength.[54][55] The risk factors with the strongest association for developing inflammatory arthritis such as rheumatoid arthritis are the female sex, a family history of rheumatoid arthritis, age, obesity, previous joint damage from an injury, and exposure to tobacco smoke.[56][57][58]
Risk factors
[edit]There are common risk factors that increase a person's chance of developing arthritis later in adulthood. Some of these are modifiable while others are not.[59] Smoking has been linked to an increased susceptibility of developing arthritis, particularly rheumatoid arthritis.[60]
Diagnosis
[edit]| Type | WBC (per mm3) | % neutrophils | Viscosity | Appearance |
|---|---|---|---|---|
| Normal | <200 | 0 | High | Transparent |
| Osteoarthritis | <5000 | <25 | High | Clear yellow |
| Trauma | <10,000 | <50 | Variable | Bloody |
| Inflammatory | 2,000–50,000 | 50–80 | Low | Cloudy yellow |
| Septic arthritis | >50,000 | >75 | Low | Cloudy yellow |
| Gonorrhea | ~10,000 | 60 | Low | Cloudy yellow |
| Tuberculosis | ~20,000 | 70 | Low | Cloudy yellow |
| Inflammatory: Arthritis, gout, rheumatoid arthritis, rheumatic fever | ||||
Diagnosis is made by clinical examination from an appropriate health professional, and may be supported by tests such as radiologic imaging and blood tests, depending on the type of suspected arthritis.[63] Pain patterns may vary depending on the type of arthritis and the location. Rheumatoid arthritis is generally worse in the morning and associated with stiffness lasting over 30 minutes.[64] On the other hand, with osteoarthritis, the pain tends to initially be related to activity and then becomes more constant over time.[65]

Important features to look out for include the following:
- Rate of onset of symptoms,
- Pattern of joint involvement,
- Symmetry of symptoms,
- Early morning stiffness,
- Associated tenderness around the joint
- Locking of joint with inactivity
- Aggravating and relieving factors, and/or
- Presence of systemic symptoms.
Physical examination may include observing the affected joints, evaluating gait, and examining the skin for findings that could be related to rheumatological disease or pulmonary inflammation. Physical examination may confirm the diagnosis or may indicate systemic disease. Chest radiographs are often used to follow progression or help assess severity.[66]
Screening blood tests for suspected arthritis include: rheumatoid factor, antinuclear factor (ANF), extractable nuclear antigen, and specific antibodies.[66]
Rheumatoid arthritis patients often have elevated erythrocyte sedimentation rate (ESR, also known as sed rate) or C-reactive protein (CRP) levels, which indicates the presence of an inflammatory process in the body.[64] Anti-cyclic citrullinated peptide (anti-CCP) antibodies and rheumatoid factor (RF) are two more common blood tests when assessing for rheumatoid arthritis.[64]
Imaging tests like X-rays are commonly utilized to diagnose and monitor arthritis.[67] Other imaging tests for rheumatoid arthritis that may be considered include computed tomography (CT) scanning, positron emission tomography (PET) scanning, bone scanning, and dual-energy X-ray absorptiometry (DEXA).[67]
Osteoarthritis
[edit]
Osteoarthritis (OA) is the most common form of arthritis.[68] It affects humans and other animals, notably dogs, but also occurs in cats and horses. It can affect both the larger (ie. knee, hip, shoulder, etc.) and the smaller joints (ie. fingers, toes, foot, etc.) of the body. The disease is caused by daily wear and tear of the joint. This process can progress more rapidly as a result of injury to the joint. Osteoarthritis is caused by the break down of the smooth surface between two bones, known as cartilage, which can eventually lead to the two opposing bones coming in direct contact and eroding one another. OA symptoms typically begin with minor pain during physical activity, but can eventually progress to be present at rest. The pain can be debilitating and prevent one from doing activities that they would normally do as part of their daily routine. OA typically affects the weight-bearing joints, such as the back, knee and hip due to the mechanical nature of this disease process. Unlike rheumatoid arthritis, osteoarthritis is most commonly a disease of the elderly. The strongest predictor of osteoarthritis is increased age, likely due to the declining ability of chondrocytes to maintain the structural integrity of cartilage.[69] More than 30 percent of women have some degree of osteoarthritis by age 65. One of the primary tools for diagnosing OA are X-rays of the joint. Findings on X-ray that are consistent with OA include those with joint space narrowing (due to cartilage breakdown), bone spurs, sclerosis, and bone cysts.[70]
Rheumatoid arthritis
[edit]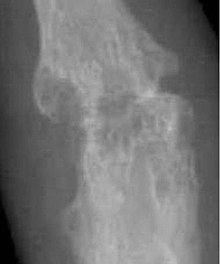
Rheumatoid arthritis (RA) is a disorder in which the body's own immune system starts to attack body tissues specifically the cartilage at the end of bones known as articular cartilage.[72] The attack is not only directed at the joint but to many other parts of the body. RA often affects joints in the fingers, wrists, knees and elbows, is symmetrical (appears on both sides of the body), and can lead to severe progressive deformity in a matter of years if not adequately treated. RA usually onsets earlier in life than OA and commonly effects people aged 20 and above. In children, the disorder can present with a skin rash, fever, pain, disability, and limitations in daily activities.[73] With earlier diagnosis and appropriate aggressive treatment, many individuals can obtain control of their symptoms leading to a better quality of life compared to those without treatment.[74][75]
One of the main triggers of bone erosion in the joints in rheumatoid arthritis is inflammation of the synovium (lining of the joint capsule), caused in part by the production of pro-inflammatory cytokines and receptor activator of nuclear factor kappa B ligand (RANKL), a cell surface protein present in Th17 cells and osteoblasts.[76] Osteoclast activity can be directly induced by osteoblasts through the RANK/RANKL mechanism.[77]

Lupus
[edit]Lupus is an autoimmune collagen vascular disorder that can be present with severe arthritis. In fact, about 90% of patients with Lupus have musculoskeletal involvement.[78] Symptoms in these patients can often mimic those of rheumatoid arthritis with similar stiffness and pain patterns. Joints in the fingers, wrist, and knee tend to be the most affected.[78] Other features commonly seen in patients with Lupus include a skin rash (pictured on the right), extreme photosensitivity, hair loss, kidney problems, and shortness of breath secondary to scarring that occurs in the lungs.[79]
Gout
[edit]
Gout is caused by deposition of uric acid crystals in the joints, which causes significant inflammation.[80] In the early stages of gout, usually only one joint is affected; however over time, many joints can become affected. Gout most commonly occurs in joints located in the big toe, knee, and/or fingers.[80] During a gout flare, the affected joints often become swollen with associated warmth and redness. The resulting pain can be significant and potentially debilitating.[81] When one of these flares occurs, management involves the use of anti-inflammatories, such as NSAIDs, colchicine, or glucocorticoids.[82] In between gout flares, it is recommended that patients take medications that decrease the production of uric acid (i.e. allopurinol, febuxostat) or increase the elimination of uric acid from the body (i.e. probenecid).[82][83]
Gout has been associated with excessive intake of alcohol and food, such as red meat.[80] Thus, it is also recommended that patients with gout adhere to a diet rich in fiber, vegetables, and whole grains, while limiting the intake of alcohol and fatty foods.[80]
There is also an uncommon form of gout that is known as pseudogout, which is caused by the formation of calcium pyrophosphate crystals in the joint.[84] Unlike gout, no targeted treatments are currently available.[84] At this time, management is aimed at decreasing inflammation in order to reduce the intensity and frequency of flares.[84]
Comparison of types
[edit]| Osteoarthritis | Rheumatoid arthritis | Gouty arthritis | |
|---|---|---|---|
| Speed of onset | Months-Years | Weeks-months[86] | Hours for an attack[87] |
| Main locations | Weight-bearing joints (such as knees, hips, vertebral column) and hands | Hands (proximal interphalangeal and metacarpophalangeal joint) wrists, ankles, knees and hips | Great toe, ankles, knees and elbows |
| Inflammation | May occur, though often mild compared to inflammation in rheumatoid arthritis | Yes | Yes |
| Radiologic changes |
|
|
|
| Laboratory findings | None | Anemia, elevated ESR and C-reactive protein (CRP), rheumatoid factor, anti-citrullinated protein antibody | Crystal in joints |
| Other features |
|
|
Other
[edit]Infectious arthritis is another severe form of arthritis that is sometimes referred to as septic arthritis. It typically occurs when a patient is ill or has an infection. Common symptoms include the sudden onset of chills, fever, and joint pain. The condition is caused by bacteria that spread through the blood stream from elsewhere in the body. This bacteria can travel to specific joints and start to erode cartilage. Infectious arthritis must be rapidly diagnosed and treated promptly in order to prevent irreversible joint damage.[88] Only about 1% of cases of infectious arthritis are a result of viruses.[89] Within recent years, the virus SARS-CoV-2, which causes Covid-19, has been added to this list.[90] SARS-CoV-2 tends to cause reactive arthritis rather than local septic arthritis.[90]
Psoriasis can develop into psoriatic arthritis.[91] With psoriatic arthritis, most individuals first develop skin symptoms (such as scaly patches and itchiness) and then begin to experience joint related symptoms. They typically experience continuous joint pain, stiffness and swelling like other forms of arthritis. This disease can go into remission, but there is currently no known cure for the disorder.[91] Treatment current revolves around decreasing autoimmune attacks with immune suppressive medications.[91] A small percentage of patients with psoriatic arthritis can develop a severely painful and destructive form of arthritis which destroys the small joints in the hands and sometimes lead to permanent disability and loss of hand function.[91]
Treatment
[edit]There is no known cure for arthritis and rheumatic diseases. Treatment options vary depending on the type of arthritis and include physical therapy, exercise and diet, orthopedic bracing, and oral and topical medications.[2][92] Joint replacement surgery may be required to repair damage, restore function, or relieve pain.[2]
Physical therapy
[edit]In general, studies have shown that physical exercise of the affected joint can noticeably improve long-term pain relief. Furthermore, exercise of the arthritic joint is encouraged to maintain the health of the particular joint and the overall body of the person.[93]
Individuals with arthritis can benefit from both physical and occupational therapy. In arthritis the joints become stiff and the range of movement can be limited. Physical therapy has been shown to significantly improve function, decrease pain, and delay the need for surgical intervention in advanced cases.[94] Exercise prescribed by a physical therapist has been shown to be more effective than medications in treating osteoarthritis of the knee. Exercise often focuses on improving muscle strength, endurance and flexibility. In some cases, exercises may be designed to train balance. Occupational therapy can provide assistance with activities. Assistive technology is a tool used to aid a person's disability by reducing their physical barriers by improving the use of their damaged body part, typically after an amputation. Assistive technology devices can be customized to the patient or bought commercially.[95]
Medications
[edit]There are several types of medications that are used for the treatment of arthritis. Treatment typically begins with medications that have the fewest side effects with further medications being added if insufficiently effective.[96]
Depending on the type of arthritis, the medications that are given may be different. For example, the first-line treatment for osteoarthritis is acetaminophen (paracetamol) while for inflammatory arthritis it involves non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen. Opioids and NSAIDs may be less well tolerated.[97] However, topical NSAIDs may have better safety profiles than oral NSAIDs. For more severe cases of osteoarthritis, intra-articular corticosteroid injections may also be considered.[98][99]
The drugs to treat rheumatoid arthritis (RA) range from corticosteroids to monoclonal antibodies given intravenously. Due to the autoimmune nature of RA, treatments may include not only pain medications and anti-inflammatory drugs, but also another category of drugs called disease-modifying antirheumatic drugs (DMARDs). csDMARDs, TNF biologics and tsDMARDs are specific kinds of DMARDs that are recommended for treatment.[100] Treatment with DMARDs is designed to slow down the progression of RA by initiating an adaptive immune response, in part by CD4+ T helper (Th) cells, specifically Th17 cells.[101] Th17 cells are present in higher quantities at the site of bone destruction in joints and produce inflammatory cytokines associated with inflammation, such as interleukin-17 (IL-17).[76]
Surgery
[edit]A number of surgical interventions have been incorporated in the treatment of arthritis since the 1950s. The primary surgical treatment option of arthritis is joint replacement surgery known as arthroplasty.[102] Common joints that are replaced due to arthritis include the shoulder, hip, and knee.[102] Arthroscopic surgery for osteoarthritis of the knee provides no additional benefit to patients when compared to optimized physical and medical therapy.[103] Joint replacement surgery can last anywhere from 15-30 years depending on the patient.[104] Following joint replacement surgery, patients can expect to get back to several physical activities including those such as swimming, tennis, and golf.[105]
Adaptive aids
[edit]People with hand arthritis can have trouble with simple activities of daily living tasks (ADLs), such as turning a key in a lock or opening jars, as these activities can be cumbersome and painful. There are adaptive aids or assistive devices (ADs) available to help with these tasks,[106] but they are generally more costly than conventional products with the same function. It is now possible to 3-D print adaptive aids, which have been released as open source hardware to reduce patient costs.[107][108] Adaptive aids can significantly help arthritis patients and the vast majority of those with arthritis need and use them.[109]
Alternative medicine
[edit]Further research is required to determine if transcutaneous electrical nerve stimulation (TENS) for knee osteoarthritis is effective for controlling pain.[110]
Low level laser therapy may be considered for relief of pain and stiffness associated with arthritis.[111] Evidence of benefit is tentative.[112]
Pulsed electromagnetic field therapy (PEMFT) has tentative evidence supporting improved functioning but no evidence of improved pain in osteoarthritis.[113] The FDA has not approved PEMFT for the treatment of arthritis. In Canada, PEMF devices are legally licensed by Health Canada for the treatment of pain associated with arthritic conditions.[114]
Epidemiology
[edit]Arthritis is predominantly a disease of the elderly, but children can also be affected by the disease.[115] Arthritis is more common in women than men at all ages and affects all races, ethnic groups and cultures. In the United States a CDC survey based on data from 2013 to 2015 showed 54.4 million (22.7%) adults had self-reported doctor-diagnosed arthritis, and 23.7 million (43.5% of those with arthritis) had arthritis-attributable activity limitation (AAAL). With an aging population, this number is expected to increase. Adults with co-morbid conditions, such as heart disease, diabetes, and obesity, were seen to have a higher than average prevalence of doctor-diagnosed arthritis (49.3%, 47.1%, and 30.6% respectively).[116]
Disability due to musculoskeletal disorders increased by 45% from 1990 to 2010. Of these, osteoarthritis is the fastest increasing major health condition.[117] Among the many reports on the increased prevalence of musculoskeletal conditions, data from Africa are lacking and underestimated. A systematic review assessed the prevalence of arthritis in Africa and included twenty population-based and seven hospital-based studies.[118] The majority of studies, twelve, were from South Africa. Nine studies were well-conducted, eleven studies were of moderate quality, and seven studies were conducted poorly. The results of the systematic review were as follows:[118]
- Rheumatoid arthritis: 0.1% in Algeria (urban setting); 0.6% in Democratic Republic of Congo (urban setting); 2.5% and 0.07% in urban and rural settings in South Africa respectively; 0.3% in Egypt (rural setting), 0.4% in Lesotho (rural setting)
- Osteoarthritis: 55.1% in South Africa (urban setting); ranged from 29.5 to 82.7% in South Africans aged 65 years and older
- Knee osteoarthritis has the highest prevalence from all types of osteoarthritis, with 33.1% in rural South Africa
- Ankylosing spondylitis: 0.1% in South Africa (rural setting)
- Psoriatic arthritis: 4.4% in South Africa (urban setting)
- Gout: 0.7% in South Africa (urban setting)
- Juvenile idiopathic arthritis: 0.3% in Egypt (urban setting)
History
[edit]Evidence of osteoarthritis and potentially inflammatory arthritis has been discovered in dinosaurs.[119][120] The first known traces of human arthritis date back as far as 4500 BC. In early reports, arthritis was frequently referred to as the most common ailment of prehistoric peoples.[121] It was noted in skeletal remains of Native Americans found in Tennessee and parts of what is now Olathe, Kansas. Evidence of arthritis has been found throughout history, from Ötzi, a mummy (c. 3000 BC) found along the border of modern Italy and Austria, to the Egyptian mummies c. 2590 BC.[122]
In 1715, William Musgrave published the second edition of his most important medical work, De arthritide symptomatica, which concerned arthritis and its effects.[123] Augustin Jacob Landré-Beauvais, a 28-year-old resident physician at Salpêtrière Asylum in France was the first person to describe the symptoms of rheumatoid arthritis. Though Landré-Beauvais' classification of rheumatoid arthritis as a relative of gout was inaccurate, his dissertation encouraged others to further study the disease.[124]
John Charnley completed the first hip replacement (total hip arthroplasty) in England to treat arthritis in the 1960s.
Society and Culture:
[edit]Arthritis is the most common cause of disability in the United States. More than 20 million individuals with arthritis have severe limitations in function on a daily basis.[12] Absenteeism and frequent visits to the physician are common in individuals who have arthritis. Arthritis can make it difficult for individuals to be physically active and some become home bound.[125] It is estimated that the total cost of arthritis cases is close to $100 billion of which almost 50% is from lost earnings.
Terminology
[edit]The term is derived from arthr- (from Ancient Greek: ἄρθρον, romanized: árthron, lit. 'joint') and -itis (from -ῖτις, -îtis, lit. 'pertaining to'), the latter suffix having come to be associated with inflammation.
The word arthritides is the plural form of arthritis, and denotes the collective group of arthritis-like conditions.[126]
See also
[edit]- Antiarthritics
- Arthritis Care (charity in the UK)
- Arthritis Foundation (US not-for-profit)
- Knee arthritis
- Osteoimmunology
- Weather pains
References
[edit]- ^ "arthritis noun - Definition, pictures, pronunciation and usage notes Oxford Advanced Learner's Dictionary". www.oxfordlearnersdictionaries.com. Retrieved 14 December 2017.
- ^ a b c d e f g h i "Arthritis and Rheumatic Diseases". NIAMS. October 2014. Archived from the original on 4 October 2016. Retrieved 31 March 2021.
- ^ a b "Arthritis Types". CDC. 22 June 2016. Archived from the original on 14 September 2016. Retrieved 14 September 2016.
- ^ "Amplified Musculoskeletal Pain Syndrome (AMPS)". Children's Health.
- ^ a b Athanasiou KA, Darling EM, Hu JC, DuRaine GD, Reddi AH (2013). Articular Cartilage. CRC Press. p. 105. ISBN 9781439853252.
- ^ a b c "Arthritis Basics". CDC. 9 May 2016. Archived from the original on 17 September 2016. Retrieved 14 September 2016.
- ^ a b c d e f g h i j "Living With Arthritis: Health Information Basics for You and Your Family". NIAMS. July 2014. Archived from the original on 4 October 2016. Retrieved 14 September 2016.
- ^ "Arthritis – Overview". mayoclinic.org. Mayo Clinic. Retrieved 6 June 2022.
- ^ a b c d "Arthritis: An Overview". OrthoInfo. October 2007. Archived from the original on 19 September 2016. Retrieved 14 September 2016.
- ^ Clegg HB, Jackson L (2013). Eating well to fight arthritis: 200 easy recipes and practical tips to help reduce inflammation and ease symptoms. Favorite Recipes Press. ISBN 978-0-9815640-5-0. OCLC 854909375.
- ^ "Traditional Chinese Medicine Formula in the Treatment of Osteoarthritis of Knees or Hips". Case Medical Research. 1 October 2019. doi:10.31525/ct1-nct04110847. ISSN 2643-4652. S2CID 242704843.
- ^ a b c d e "Arthritis". CDC. 22 July 2015. Archived from the original on 22 September 2016. Retrieved 14 September 2016.
- ^ SIDE EFFECTS MAY INCLUDE STRANGERS, McGill-Queen's University Press, 22 October 2020, p. 27, doi:10.2307/j.ctv1ghv4jh.24, S2CID 243669150
- ^ "Blood-pressure pill may also aid weight loss". New Scientist. 198 (2654): 16. May 2008. doi:10.1016/s0262-4079(08)61076-3. ISSN 0262-4079.
- ^ "Higher-than-recommended doses of antipsychotic medications may not benefit people with schizophrenia and may increase side effects". PsycEXTRA Dataset. 2007. doi:10.1037/e603782007-025.
- ^ March L, Smith EU, Hoy DG, Cross MJ, Sanchez-Riera L, Blyth F, et al. (June 2014). "Burden of disability due to musculoskeletal (MSK) disorders". Best Practice & Research. Clinical Rheumatology. 28 (3): 353–366. doi:10.1016/j.berh.2014.08.002. PMID 25481420.
- ^ "National Health Survey". ABS. 8 December 2015. Archived from the original on 16 January 2017. Retrieved 14 January 2017.
- ^ Pirotta M (September 2010). "Arthritis disease - the use of complementary therapies". Australian Family Physician. 39 (9): 638–640. PMID 20877766.
- ^ Waite M, ed. (2012). Paperback Oxford English Dictionary. Oxford: Oxford University Press. p. 35. ISBN 9780199640942. Archived from the original on 20 December 2016.
- ^ Leonard C (2015). Quick & Easy Medical Terminology - E-Book. Elsevier Health Sciences. p. 160. ISBN 9780323370646.
- ^ "Osteoarthritis". The Lecturio Medical Concept Library. Retrieved 22 August 2021.
- ^ "Rheumatoid Arthritis". The Lecturio Medical Concept Library. Retrieved 22 August 2021.
- ^ "Gout". The Lecturio Medical Concept Library. 9 September 2020. Retrieved 22 August 2021.
- ^ "Septic Arthritis". The Lecturio Medical Concept Library. Retrieved 22 August 2021.
- ^ "Ankylosing Spondylitis". The Lecturio Medical Concept Library. Retrieved 22 August 2021.
- ^ Prakken B, Albani S, Martini A (June 2011). "Juvenile idiopathic arthritis". Lancet. 377 (9783): 2138–2149. doi:10.1016/S0140-6736(11)60244-4. PMID 21684384. S2CID 202802455.
- ^ Akkara Veetil BM, Yee AH, Warrington KJ, Aksamit AJ, Mason TG (December 2012). "Aseptic meningitis in adult onset Still's disease". Rheumatology International. 32 (12): 4031–4034. doi:10.1007/s00296-010-1529-8. PMID 20495923. S2CID 19431424.
- ^ Garrick N (14 April 2017). "Psoriatic Arthritis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. Retrieved 24 November 2021.
- ^ "Questions and Answers About Psoriasis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. 12 April 2017. Archived from the original on 22 April 2017. Retrieved 22 April 2017.
- ^ American College of Rheumatology. "Reactive Arthritis". Retrieved 24 January 2017.
- ^ "Ehlers-Danlos Syndrome". The Lecturio Medical Concept Library. Retrieved 22 August 2021.
- ^ McDowell LA, Kudaravalli P, Sticco KL (2021). "Iron Overload". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30252387. Retrieved 24 November 2021.
- ^ "Hepatitis". MedlinePlus. 20 May 2020. Retrieved 19 July 2020.
Your liver is the largest organ inside your body. It helps your body digest food, store energy, and remove poisons. Hepatitis is an inflammation of the liver.
- ^ "Hepatitis". NIAID. Archived from the original on 4 November 2016. Retrieved 2 November 2016.
- ^ "Lyme Disease". The Lecturio Medical Concept Library. Retrieved 22 August 2021.
- ^ "What Is Sjögren's Syndrome? Fast Facts". NIAMS. November 2014. Archived from the original on 4 July 2016. Retrieved 15 July 2016.
- ^ "Hashimoto's Thyroiditis". The Lecturio Medical Concept Library. Retrieved 22 August 2021.
- ^ Guandalini S, Assiri A (March 2014). "Celiac disease: a review". JAMA Pediatrics. 168 (3): 272–278. doi:10.1001/jamapediatrics.2013.3858. PMID 24395055.
- ^ Fasano A, Sapone A, Zevallos V, Schuppan D (May 2015). "Nonceliac gluten sensitivity". Gastroenterology. 148 (6): 1195–1204. doi:10.1053/j.gastro.2014.12.049. PMID 25583468.
- ^ Volta U, Caio G, De Giorgio R, Henriksen C, Skodje G, Lundin KE (June 2015). "Non-celiac gluten sensitivity: a work-in-progress entity in the spectrum of wheat-related disorders". Best Practice & Research. Clinical Gastroenterology. 29 (3): 477–491. doi:10.1016/j.bpg.2015.04.006. PMID 26060112.
- ^ Catassi C, Bai JC, Bonaz B, Bouma G, Calabrò A, Carroccio A, et al. (September 2013). "Non-Celiac Gluten sensitivity: the new frontier of gluten related disorders". Nutrients (Review). 5 (10): 3839–3853. doi:10.3390/nu5103839. PMC 3820047. PMID 24077239.
- ^ "Crohn's Disease". The Lecturio Medical Concept Library. 28 August 2020. Retrieved 22 August 2021.
- ^ "Ulcerative Colitis". The Lecturio Medical Concept Library. 26 August 2020. Retrieved 22 August 2021.
- ^ "Henoch-Schönlein Purpura". The Lecturio Medical Concept Library. Retrieved 22 August 2021.
- ^ "Sarcoidosis". The Lecturio Medical Concept Library. Retrieved 22 August 2021.
- ^ "Whipple's Disease". The Lecturio Medical Concept Library. Retrieved 22 August 2021.
- ^ Rezaei N (November 2006). "TNF-receptor-associated periodic syndrome (TRAPS): an autosomal dominant multisystem disorder". Clinical Rheumatology. 25 (6): 773–777. doi:10.1007/s10067-005-0198-6. PMID 16447098. S2CID 41808394.subscription needed
- ^ James W, Berger T, Elston D (2005). Andrews' Diseases of the Skin: Clinical Dermatology (10th ed.). Saunders. ISBN 0-7216-2921-0.
- ^ "Systemic Lupus Erythematosus". The Lecturio Medical Concept Library. Retrieved 22 August 2021.
- ^ Wollenhaupt J, Zeidler H (July 1998). "Undifferentiated arthritis and reactive arthritis". Current Opinion in Rheumatology. 10 (4): 306–313. doi:10.1097/00002281-199807000-00005. PMID 9725091.
- ^ Swash M, Glynn M, eds. (2007). Hutchison's Clinical Methods: An Integrated Approach to Clinical Practice (22nd ed.). Edinburgh: Saunders Elsevier. ISBN 978-0702027994.
- ^ Eustice C (2012). Arthritis: types of arthritis. Adams Media. ISBN 978-1-4405-4446-0. OCLC 808835849.
- ^ Galloway JB, Scott DL (December 2017). "Management of common types of arthritis in older adults". Oxford Textbook of Geriatric Medicine. Oxford University Press. pp. 577–584. doi:10.1093/med/9780198701590.003.0075. ISBN 978-0-19-870159-0.
- ^ Vina ER, Kwoh CK (March 2018). "Epidemiology of Osteoarthritis: Literature Update". Current Opinion in Rheumatology. 30 (2): 160–167. doi:10.1097/BOR.0000000000000479. ISSN 1040-8711. PMC 5832048. PMID 29227353.
- ^ Christensen R, Bartels EM, Astrup A, Bliddal H (April 2007). "Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: a systematic review and meta-analysis". Annals of the Rheumatic Diseases. 66 (4): 433–439. doi:10.1136/ard.2006.065904. ISSN 0003-4967. PMC 1856062. PMID 17204567.
- ^ Chauhan K, Jandu JS, Brent LH, Al-Dhahir MA (2025), "Rheumatoid Arthritis", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 28723028, retrieved 24 January 2025
- ^ Deane KD, Demoruelle MK, Kelmenson LB, Kuhn KA, Norris JM, Holers VM (February 2017). "Genetic and environmental risk factors for rheumatoid arthritis". Best Practice & Research. Clinical Rheumatology. 31 (1): 3–18. doi:10.1016/j.berh.2017.08.003. PMC 5726551. PMID 29221595.
- ^ "Arthritis - Risk factors". mayoclinic.org. Mayo Clinic.
- ^ "Arthritis Risk Factors". Centers for Disease Control and Prevention. 17 June 2020. Retrieved 22 November 2020.
- ^ "Smoking and Rheumatoid Arthritis". NRAS. National Rheumatoid Arthritis Society. Retrieved 20 November 2020.
- ^ Flynn JA, Choi MJ, Wooster DL (2013). Oxford American Handbook of Clinical Medicine. US: OUP. p. 400. ISBN 978-0-19-991494-4.
- ^ Seidman AJ, Limaiem F (2019). "Synovial Fluid Analysis". StatPearls. StatPearls Publishing. PMID 30725799. Retrieved 19 December 2019.
- ^ "How is arthritis diagnosed? | Arthritis Research UK". www.arthritisresearchuk.org. Archived from the original on 2 April 2015. Retrieved 9 June 2015.
- ^ a b c Garrick N (20 April 2017). "Rheumatoid Arthritis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. Retrieved 6 May 2019.
- ^ Yu H, Huang T, Lu WW, Tong L, Chen D (22 April 2022). "Osteoarthritis Pain". International Journal of Molecular Sciences. 23 (9): 4642. doi:10.3390/ijms23094642. ISSN 1422-0067. PMC 9105801. PMID 35563035.
- ^ a b Davis JL, Murray JF (2016). "History and Physical Examination". Murray and Nadel's Textbook of Respiratory Medicine: 263–277.e2. doi:10.1016/B978-1-4557-3383-5.00016-6. ISBN 978-1-4557-3383-5. PMC 7152492.
- ^ a b "Rheumatoid arthritis - Diagnosis". nhs.uk. 23 October 2017.
- ^ VanItallie TB (October 2010). "Gout: epitome of painful arthritis". Metabolism. 59 (Suppl 1): S32 – S36. doi:10.1016/j.metabol.2010.07.009. PMID 20837191.
- ^ Pereira D, Ramos E, Branco J (January 2015). "Osteoarthritis". Acta Médica Portuguesa. 28 (1): 99–106. doi:10.20344/amp.5477. PMID 25817486.
- ^ Fan Z, Yan L, Liu H, Li X, Fan K, Liu Q, Li JJ, Wang B (29 March 2023). "The prevalence of hip osteoarthritis: a systematic review and meta-analysis". Arthritis Research & Therapy. 25 (1): 51. doi:10.1186/s13075-023-03033-7. ISSN 1478-6362. PMC 10053484. PMID 36991481.
- ^ Ideguchi H, Ohno S, Hattori H, Senuma A, Ishigatsubo Y (2006). "Bone erosions in rheumatoid arthritis can be repaired through reduction in disease activity with conventional disease-modifying antirheumatic drugs". Arthritis Research & Therapy. 8 (3): R76. doi:10.1186/ar1943. PMC 1526642. PMID 16646983.
- ^ "Rheumatoid Arthritis (RA) | Arthritis". www.cdc.gov. 5 March 2019. Retrieved 6 May 2019.
- ^ "Frequently Asked Questions (FAQs) about Arthritis | CDC". www.cdc.gov. 21 February 2019. Retrieved 6 May 2019.
- ^ "What Is Rheumatoid Arthritis? Symptoms And Treatment". familydoctor.org. Retrieved 6 May 2019.
- ^ Donahue KE, Gartlehner G, Schulman ER, Jonas B, Coker-Schwimmer E, Patel SV, Weber RP, Lohr KN, Bann C (2018). Drug Therapy for Early Rheumatoid Arthritis: A Systematic Review Update (Report). Agency for Healthcare Research and Quality (AHRQ). doi:10.23970/ahrqepccer211.
- ^ a b Chabaud M, Garnero P, Dayer JM, Guerne PA, Fossiez F, Miossec P (July 2000). "Contribution of interleukin 17 to synovium matrix destruction in rheumatoid arthritis". Cytokine. 12 (7): 1092–1099. doi:10.1006/cyto.2000.0681. PMID 10880256.
- ^ Won HY, Lee JA, Park ZS, Song JS, Kim HY, Jang SM, et al. (March 2011). "Prominent bone loss mediated by RANKL and IL-17 produced by CD4+ T cells in TallyHo/JngJ mice". PLOS ONE. 6 (3): e18168. Bibcode:2011PLoSO...618168W. doi:10.1371/journal.pone.0018168. PMC 3064589. PMID 21464945.
- ^ a b Ceccarelli F, Govoni M, Piga M, Cassone G, Cantatore FP, Olivieri G, Cauli A, Favalli EG, Atzeni F, Gremese E, Iannone F, Caporali R, Sebastiani M, Ferraccioli GF, Lapadula G (12 October 2022). "Arthritis in Systemic Lupus Erythematosus: From 2022 International GISEA/OEG Symposium". Journal of Clinical Medicine. 11 (20): 6016. doi:10.3390/jcm11206016. ISSN 2077-0383. PMC 9604412. PMID 36294337.
- ^ Rheumatoid Arthritis: Differential Diagnoses & Workup~diagnosis at eMedicine
- ^ a b c d Zhang Y, Chen S, Yuan M, Xu Y, Xu H (26 August 2022). "Gout and Diet: A Comprehensive Review of Mechanisms and Management". Nutrients. 14 (17): 3525. doi:10.3390/nu14173525. ISSN 2072-6643. PMC 9459802. PMID 36079783.
- ^ Becker MA (2005). Arthritis and Allied Conditions: A textbook of Rheumatology edition 15. Lippincott Williams & Wilkins. pp. 2303–2339.
- ^ a b Afinogenova Y, Danve A, Neogi T (1 March 2022). "Update on Gout Management: what's old and what's new". Current Opinion in Rheumatology. 34 (2): 118–124. doi:10.1097/BOR.0000000000000861. ISSN 1040-8711. PMC 8799507. PMID 34907116.
- ^ Ali S, Lally EV (November 2009). "Treatment failure gout". Medicine and Health, Rhode Island. 92 (11): 369–371. CiteSeerX 10.1.1.608.3812. PMID 19999896.
- ^ a b c Stack J, McCarthy G (1 December 2021). "Calcium pyrophosphate deposition (CPPD) disease – Treatment options". Best Practice & Research Clinical Rheumatology. Crystal Induced Arthritis. 35 (4): 101720. doi:10.1016/j.berh.2021.101720. ISSN 1521-6942. PMID 34756508.
- ^ Unless otherwise specified in table box, the reference is: Agabegi ED, Agabegi SS (2008). "Table 6–7". Step-Up to Medicine. Step-Up Series. Hagerstwon MD: Lippincott Williams & Wilkins. p. 253. ISBN 978-0-7817-7153-5.
- ^ Diagnosis lag time of median 4 weeks, and median diagnosis lag time of 18 weeks, taken from: Chan KW, Felson DT, Yood RA, Walker AM (June 1994). "The lag time between onset of symptoms and diagnosis of rheumatoid arthritis". Arthritis and Rheumatism. 37 (6): 814–820. doi:10.1002/art.1780370606. PMID 8003053.
- ^ Schaider J, Wolfson AB, Hendey GW, Ling L, Rosen CL (2009). Harwood-Nuss' Clinical Practice of Emergency Medicine (Clinical Practice of Emergency Medicine (Harwood-Nuss)). Hagerstwon, MD: Lippincott Williams & Wilkins. pp. 740 (upper right of page). ISBN 978-0-7817-8943-1. Archived from the original on 21 March 2015.
- ^ "Severe Arthritis Disease Facts". Arthritis.org. Archived from the original on 23 April 2007. Retrieved 5 February 2010.
- ^ Marks M, Marks JL (2016). "Viral arthritis". Clinical Medicine. 16 (2): 129–134. doi:10.7861/clinmedicine.16-2-129. PMC 4868140. PMID 27037381.
- ^ a b Slouma M, Abbes M, Louzir B (2023). "Reactive arthritis occurring after COVID-19 infection: a narrative review". Infection. 51 (1): 37–45. doi:10.1007/s15010-022-01858-z. PMC 9162104. PMID 35655110.
- ^ a b c d "Psoriatic Arthritis". Mayo Clinic. Archived from the original on 9 February 2010. Retrieved 5 February 2010.
- ^ "Knee braces for osteoarthritis - Mayo Clinic". www.mayoclinic.org. Retrieved 31 March 2021.
- ^ Ettinger WH, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. (January 1997). "A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST)". JAMA. 277 (1): 25–31. doi:10.1001/jama.1997.03540250033028. PMID 8980206.
- ^ Fransen M, Crosbie J, Edmonds J (January 2001). "Physical therapy is effective for patients with osteoarthritis of the knee: a randomized controlled clinical trial". The Journal of Rheumatology. 28 (1): 156–164. PMID 11196518.
- ^ "The Role of Occupational Therapy in Providing Assistive Technology Devices and Services". www.aota.org. 2018. Retrieved 8 April 2018.
- ^ "Arthritis Drugs". arthritistoday.org. Archived from the original on 22 July 2010. Retrieved 5 July 2010.
- ^ Reid MC, Shengelia R, Parker SJ (March 2012). "Pharmacologic management of osteoarthritis-related pain in older adults". The American Journal of Nursing. 112 (3 Suppl 1): S38 – S43. doi:10.1097/01.NAJ.0000412650.02926.e3. PMC 3733545. PMID 22373746.
- ^ McAlindon TE, LaValley MP, Harvey WF, Price LL, Driban JB, Zhang M, Ward RJ (16 May 2017). "Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial". JAMA. 317 (19): 1967–1975. doi:10.1001/jama.2017.5283. ISSN 0098-7484. PMC 5815012. PMID 28510679.
- ^ Taruc-Uy RL, Lynch SA (December 2013). "Diagnosis and treatment of osteoarthritis". Primary Care. 40 (4): 821–36, vii. doi:10.1016/j.pop.2013.08.003. PMID 24209720. S2CID 43061687.
- ^ Donahue KE, Schulman ER, Gartlehner G, Jonas BL, Coker-Schwimmer E, Patel SV, et al. (October 2019). "Comparative Effectiveness of Combining MTX with Biologic Drug Therapy Versus Either MTX or Biologics Alone for Early Rheumatoid Arthritis in Adults: a Systematic Review and Network Meta-analysis". Journal of General Internal Medicine. 34 (10): 2232–2245. doi:10.1007/s11606-019-05230-0. PMC 6816735. PMID 31388915.
- ^ Kurebayashi Y, Nagai S, Ikejiri A, Koyasu S (April 2013). "Recent advances in understanding the molecular mechanisms of the development and function of Th17 cells". Genes to Cells. 18 (4): 247–265. doi:10.1111/gtc.12039. PMC 3657121. PMID 23383714.
- ^ a b Park J, Chang MJ, Kim TW, D’Lima Darryl D., Kim H, Han HS (4 December 2024). "Serial changes in patient-reported outcome measures and satisfaction rate during long-term follow-up after total knee arthroplasty: a systematic review and meta-analysis". Knee Surgery & Related Research. 36 (1): 43. doi:10.1186/s43019-024-00241-6. ISSN 2234-2451. PMC 11616191. PMID 39633483.
{{cite journal}}: Vancouver style error: non-Latin character in name 4 (help) - ^ Kirkley A, Birmingham TB, Litchfield RB, Giffin JR, Willits KR, Wong CJ, et al. (September 2008). "A randomized trial of arthroscopic surgery for osteoarthritis of the knee". The New England Journal of Medicine. 359 (11): 1097–1107. doi:10.1056/NEJMoa0708333. PMID 18784099.
- ^ Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR (February 2019). "How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up". The Lancet. 393 (10172): 655–663. doi:10.1016/S0140-6736(18)32531-5. PMC 6381229. PMID 30782341.
- ^ Liu JN, Steinhaus ME, Garcia GH, Chang B, Fields K, Dines DM, Warren RF, Gulotta LV (January 2018). "Return to sport after shoulder arthroplasty: a systematic review and meta-analysis". Knee Surgery, Sports Traumatology, Arthroscopy. 26 (1): 100–112. doi:10.1007/s00167-017-4547-1. ISSN 0942-2056. PMID 28409200.
- ^ "10 Terrific Arthritis Gadgets - Arthritis Center - Everyday Health". EverydayHealth.com. 5 February 2013. Retrieved 8 March 2019.
- ^ "3-D Printing Offers Helping Hand to People with Arthritis". OrthoFeed. 15 December 2018. Archived from the original on 15 November 2020. Retrieved 8 March 2019.
- ^ Gallup N, Bow JK, Pearce JM (December 2018). "Economic Potential for Distributed Manufacturing of Adaptive Aids for Arthritis Patients in the U.S". Geriatrics. 3 (4): 89. doi:10.3390/geriatrics3040089. PMC 6371113. PMID 31011124.
- ^ Yeung KT, Lin CH, Teng YL, Chen FF, Lou SZ, Chen CL (29 March 2016). "Use of and Self-Perceived Need for Assistive Devices in Individuals with Disabilities in Taiwan". PLOS ONE. 11 (3): e0152707. Bibcode:2016PLoSO..1152707Y. doi:10.1371/journal.pone.0152707. PMC 4811424. PMID 27023276.
- ^ Rutjes AW, Nüesch E, Sterchi R, Kalichman L, Hendriks E, Osiri M, et al. (October 2009). "Transcutaneous electrostimulation for osteoarthritis of the knee". The Cochrane Database of Systematic Reviews. 2009 (4): CD002823. doi:10.1002/14651858.CD002823.pub2. PMC 7120411. PMID 19821296.
- ^ Brosseau L, Welch V, Wells G, Tugwell P, de Bie R, Gam A, et al. (August 2000). "Low level laser therapy for osteoarthritis and rheumatoid arthritis: a metaanalysis". The Journal of Rheumatology. 27 (8): 1961–1969. PMID 10955339.
- ^ Brosseau L, Robinson V, Wells G, Debie R, Gam A, Harman K, et al. (October 2005). "Low level laser therapy (Classes I, II and III) for treating rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2005 (4): CD002049. doi:10.1002/14651858.CD002049.pub2. PMC 8406947. PMID 16235295.
- ^ Vavken P, Arrich F, Schuhfried O, Dorotka R (May 2009). "Effectiveness of pulsed electromagnetic field therapy in the management of osteoarthritis of the knee: a meta-analysis of randomized controlled trials". Journal of Rehabilitation Medicine. 41 (6): 406–411. doi:10.2340/16501977-0374. PMID 19479151.
- ^ "Medical Devices Active Licence Listing (MDALL)". Health Canada. 16 July 2002. Retrieved 28 March 2020.
- ^ "Juvenile idiopathic arthritis: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 6 May 2019.
- ^ Barbour KE, Helmick CG, Boring M, Brady TJ (March 2017). "Vital Signs: Prevalence of Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation - United States, 2013-2015". MMWR. Morbidity and Mortality Weekly Report. 66 (9): 246–253. doi:10.15585/mmwr.mm6609e1. PMC 5687192. PMID 28278145.
- ^ GBD 2010 Country Collaboration (March 2013). "GBD 2010 country results: a global public good". Lancet. 381 (9871): 965–970. doi:10.1016/S0140-6736(13)60283-4. PMID 23668561. S2CID 11808683.
- ^ a b Usenbo A, Kramer V, Young T, Musekiwa A (4 August 2015). "Prevalence of Arthritis in Africa: A Systematic Review and Meta-Analysis". PLOS ONE. 10 (8): e0133858. Bibcode:2015PLoSO..1033858U. doi:10.1371/journal.pone.0133858. PMC 4524637. PMID 26241756.
- ^ DeLisa JA, Gans BM, Walsh NE (2005). Physical Medicine and Rehabilitation: Principles and Practice. Lippincott Williams & Wilkins. pp. 765–. ISBN 978-0-7817-4130-9. Archived from the original on 8 January 2017.
- ^ Blumberg BS, Sokoloff L (December 1961). "Coalescence of caudal vertebrae in the giant dinosaur Diplodocus". Arthritis and Rheumatism. 4 (6): 592–601. doi:10.1002/art.1780040605. PMID 13870231.
- ^ Bridges PS (1992). "Prehistoric Arthritis in the Americas". Annual Review of Anthropology. 21: 67–91. doi:10.1146/annurev.an.21.100192.000435.
- ^ "Arthritis History". Medical News. 2 December 2009. Archived from the original on 30 January 2010.
- ^ Cameron A (September 2004). "Musgrave, William (1655–1721)". Oxford Dictionary of National Biography. Oxford University Press.
- ^ Entezami P, Fox DA, Clapham PJ, Chung KC (February 2011). "Historical perspective on the etiology of rheumatoid arthritis". Hand Clinics. 27 (1): 1–10. doi:10.1016/j.hcl.2010.09.006. PMC 3119866. PMID 21176794.
- ^ MUTTER DJ (21 November 2023). "Ask the Expert | What medical conditions most commonly cause older adults to become homebound?". The Daily Progress. Retrieved 20 April 2024.
- ^ "Definition of ARTHRITIDES". www.merriam-webster.com. Retrieved 5 November 2020.
External links
[edit]- American College of Rheumatology – US professional society of rheumatologists
- National Institute of Arthritis and Musculoskeletal and Skin Diseases - US National Institute of Arthritis and Musculoskeletal and Skin Diseases
- The Ultimate Arthritis Diet Arthritis Foundation