| BCHE | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | BCHE, CHE1, CHE2, E1, butyrylcholinesterase, BCHED | ||||||||||||||||||||||||||||||||||||||||||||||||||
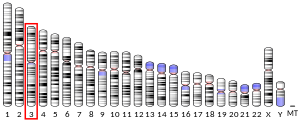
| External IDs | OMIM: 177400; MGI: 894278; HomoloGene: 20065; GeneCards: BCHE; OMA:BCHE - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
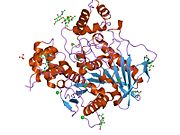
Butyrylcholinesterase (HGNC symbol BCHE; EC 3.1.1.8), also known as BChE, BuChE, BuChase, pseudocholinesterase, or plasma (cholin)esterase,[5] is a nonspecific cholinesterase enzyme that hydrolyses many different choline-based esters. In humans, it is made in the liver, found mainly in blood plasma, and encoded by the BCHE gene.[6]
It is very similar to the neuronal acetylcholinesterase, which is also known as RBC or erythrocyte cholinesterase.[5] The term "serum cholinesterase" is generally used in reference to a clinical test that reflects levels of both of these enzymes in the blood.[5] Assay of butyrylcholinesterase activity in plasma can be used as a liver function test as both hypercholinesterasemia and hypocholinesterasemia indicate pathological processes. The half-life of BCHE is approximately 10 to 14 days.[7]
Butyrylcholine is a synthetic compound that does not occur in the body naturally. It is used as a tool to distinguish between acetylcholinesterase and butyrylcholinesterase.
Potential physiological role
[edit]Butyrylcholinesterase may be a physiological ghrelin regulator.[8]
Clinical significance
[edit]Pseudocholinesterase deficiency results in delayed metabolism of only a few compounds of clinical significance, including the following: succinylcholine, mivacurium, procaine, heroin, and cocaine. Of these, its most clinically important substrate is the depolarizing neuromuscular blocking agent, succinylcholine, which the pseudocholinesterase enzyme hydrolyzes to succinylmonocholine and then to succinic acid.[citation needed]
In individuals with normal plasma levels of normally functioning pseudocholinesterase enzyme, hydrolysis and inactivation of approximately 90–95% of an intravenous dose of succinylcholine occurs before it reaches the neuromuscular junction. The remaining 5–10% of the succinylcholine dose acts as an acetylcholine receptor agonist at the neuromuscular junction, causing prolonged depolarization of the postsynaptic junction of the motor-end plate. This depolarization initially triggers fasciculation of skeletal muscle. As a result of prolonged depolarization, endogenous acetylcholine released from the presynaptic membrane of the motor neuron does not produce any additional change in membrane potential after binding to its receptor on the myocyte. Flaccid paralysis of skeletal muscles develops within one minute. In normal subjects, skeletal muscle function returns to normal approximately five minutes after a single bolus injection of succinylcholine as it passively diffuses away from the neuromuscular junction. Pseudocholinesterase deficiency can result in higher levels of intact succinylcholine molecules reaching receptors in the neuromuscular junction, causing the duration of paralytic effect to continue for as long as eight hours. This condition is recognized clinically when paralysis of the respiratory and other skeletal muscles fails to spontaneously resolve after succinylcholine is administered as an adjunctive paralytic agent during anesthesia procedures. In such cases respiratory assistance is required.[9]
Mutant alleles at the BCHE locus are responsible for suxamethonium sensitivity. Homozygous persons sustain prolonged apnea after administration of the muscle relaxant suxamethonium in connection with surgical anesthesia. The activity of pseudocholinesterase in the serum is low and its substrate behavior is atypical. In the absence of the relaxant, the homozygote is at no known disadvantage.[10]
Finally, pseudocholinesterase metabolism of procaine results in formation of paraaminobenzoic acid (PABA). If the patient receiving procaine is on sulfonamide antibiotics such as bactrim the antibiotic effect will be antagonized by providing a new source of PABA to the microbe for subsequent synthesis of folic acid.[citation needed]
Prophylactic countermeasure against nerve agents
[edit]Butyrylcholinesterase is a prophylactic countermeasure against organophosphate nerve agents. It binds nerve agent in the bloodstream before it can exert effects in the nervous system. Because it is a biological scavenger (and universal target), it is currently the only therapeutic agent effective in providing complete stoichiometric protection against the entire spectrum of organophosphate nerve agents.[11]
Prophylactic against cocaine addiction
[edit]An experimental new drug was developed for the potential treatment of cocaine abuse and overdose based on the pseudocholinesterase structure (it was a human BChE mutant with improved catalytic efficiency). It was shown to remove cocaine from the body 2000 times as fast as the natural form of BChE. Studies in rats have shown that the drug prevented convulsions and death when administered cocaine overdoses.[12]
Transplantation of skin cells modified to express the enhanced form of butyrylcholinesterase into mice enables the long-term release of the enzyme and efficiently protects the mice from cocaine-seeking behavior and cocaine overdose.[13]
Marker for risk of SIDS
[edit]Research published by the SIDS and Sleep Apnoea Research Group of The Children's Hospital in Westmead, New South Wales, Australia, in the May 6, 2022 edition of in The Lancet indicates that BChE may be a marker for babies that are at risk of sudden infant death syndrome (SIDS). That is, lower levels of BChE were associated with an increased risk of SIDS.[14]
Interactive pathway map
[edit]Click on genes, proteins and metabolites below to link to respective articles. [§ 1]
- ^ The interactive pathway map can be edited at WikiPathways: "IrinotecanPathway_WP229".
Inhibitors
[edit]- Phytocannabinoids[15]
- Cymserine and derivatives
- Profenamine
- Rivastigmine
- Tacrine
- (+)-ZINC-12613047: IC50 human BChE 13nM, high selectivity over AChE.[16]
- Hybrid/bitopic ligands[17]
Nomenclature
[edit]The nomenclatural variations of BCHE and of cholinesterases generally are discussed at Cholinesterase § Types and nomenclature.
See also
[edit]References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000114200 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000027792 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b c Jasmin L (2013-05-28). "Cholinesterase - blood". University of Maryland Medical Center. Archived from the original on 2012-10-30. Retrieved 2011-09-07.
- ^ Allderdice PW, Gardner HA, Galutira D, Lockridge O, LaDu BN, McAlpine PJ (October 1991). "The cloned butyrylcholinesterase (BCHE) gene maps to a single chromosome site, 3q26". Genomics. 11 (2): 452–454. doi:10.1016/0888-7543(91)90154-7. hdl:2027.42/29109. PMID 1769657.
- ^ Whittaker M (February 1980). "Plasma cholinesterase variants and the anaesthetist". Anaesthesia. 35 (2): 174–197. doi:10.1111/j.1365-2044.1980.tb03800.x. PMID 6992635. S2CID 32806785.
- ^ Chen VP, Gao Y, Geng L, Parks RJ, Pang YP, Brimijoin S (February 2015). "Plasma butyrylcholinesterase regulates ghrelin to control aggression". Proceedings of the National Academy of Sciences of the United States of America. 112 (7): 2251–2256. Bibcode:2015PNAS..112.2251C. doi:10.1073/pnas.1421536112. PMC 4343161. PMID 25646463.
- ^ "Pseudocholinesterase Deficiency". Medscape. WebMD LLC. 15 July 2021.
- ^ "Entrez Gene: BCHE butyrylcholinesterase".
- ^ "Medical Identification and Treatment Systems(MITS)". Joint Program Executive Office for Chemical and Biological Defense. United States Army. Archived from the original on 2016-10-28. Retrieved 2014-08-13.
- ^ Zheng F, Yang W, Ko MC, Liu J, Cho H, Gao D, et al. (September 2008). "Most efficient cocaine hydrolase designed by virtual screening of transition states". Journal of the American Chemical Society. 130 (36): 12148–12155. doi:10.1021/ja803646t. PMC 2646118. PMID 18710224.
- "Potential New Drug For Cocaine Addiction And Overdose". ScienceDaily (Press release). September 16, 2008.
- ^ Li Y, Kong Q, Yue J, Gou X, Xu M, Wu X (February 2019). "Genome-edited skin epidermal stem cells protect mice from cocaine-seeking behaviour and cocaine overdose". Nature Biomedical Engineering. 3 (2): 105–113. doi:10.1038/s41551-018-0293-z. PMC 6423967. PMID 30899600.
- ^ Harrington CT, Hafid NA, Waters KA (June 2022). "Butyrylcholinesterase is a potential biomarker for Sudden Infant Death Syndrome". eBioMedicine. 80. The Children's Hospital in Westmead, New South Wales, Australia: 104041. doi:10.1016/j.ebiom.2022.104041. PMC 9092508. PMID 35533499. S2CID 248645079.
- ^ Puopolo T, Liu C, Ma H, Seeram NP (2022-04-19). "Inhibitory Effects of Cannabinoids on Acetylcholinesterase and Butyrylcholinesterase Enzyme Activities". Medical Cannabis and Cannabinoids. 5 (1): 85–94. doi:10.1159/000524086. PMC 9149358. PMID 35702400.
- ^ Brus B, Košak U, Turk S, Pišlar A, Coquelle N, Kos J, et al. (October 2014). "Discovery, biological evaluation, and crystal structure of a novel nanomolar selective butyrylcholinesterase inhibitor". Journal of Medicinal Chemistry. 57 (19): 8167–8179. doi:10.1021/jm501195e. PMID 25226236.
- ^ Messerer R, Dallanoce C, Matera C, Wehle S, Flammini L, Chirinda B, et al. (June 2017). "Novel bipharmacophoric inhibitors of the cholinesterases with affinity to the muscarinic receptors M1 and M2". MedChemComm. 8 (6): 1346–1359. doi:10.1039/c7md00149e. PMC 6072511. PMID 30108847.
Further reading
[edit]- Bodur E, Cokugras AN (December 2005). "The effects of indole-3-acetic acid on human and horse serum butyrylcholinesterase". Chemico-Biological Interactions. 157–158 (16): 375–378. doi:10.1016/j.cbi.2005.10.061. PMID 16429500.
- Lockridge O (October 1988). "Structure of human serum cholinesterase". BioEssays. 9 (4): 125–128. doi:10.1002/bies.950090406. hdl:2027.42/50189. PMID 3067729. S2CID 29779511.
- Allderdice PW, Gardner HA, Galutira D, Lockridge O, LaDu BN, McAlpine PJ (October 1991). "The cloned butyrylcholinesterase (BCHE) gene maps to a single chromosome site, 3q26". Genomics. 11 (2): 452–454. doi:10.1016/0888-7543(91)90154-7. hdl:2027.42/29109. PMID 1769657.
- Gaughan G, Park H, Priddle J, Craig I, Craig S (October 1991). "Refinement of the localization of human butyrylcholinesterase to chromosome 3q26.1-q26.2 using a PCR-derived probe". Genomics. 11 (2): 455–458. doi:10.1016/0888-7543(91)90155-8. PMID 1769658.
- Arpagaus M, Kott M, Vatsis KP, Bartels CF, La Du BN, Lockridge O (January 1990). "Structure of the gene for human butyrylcholinesterase. Evidence for a single copy". Biochemistry. 29 (1): 124–131. doi:10.1021/bi00453a015. PMID 2322535.
- Nogueira CP, McGuire MC, Graeser C, Bartels CF, Arpagaus M, Van der Spek AF, et al. (May 1990). "Identification of a frameshift mutation responsible for the silent phenotype of human serum cholinesterase, Gly 117 (GGT----GGAG)". American Journal of Human Genetics. 46 (5): 934–942. PMC 1683584. PMID 2339692.
- McGuire MC, Nogueira CP, Bartels CF, Lightstone H, Hajra A, Van der Spek AF, et al. (February 1989). "Identification of the structural mutation responsible for the dibucaine-resistant (atypical) variant form of human serum cholinesterase". Proceedings of the National Academy of Sciences of the United States of America. 86 (3): 953–957. Bibcode:1989PNAS...86..953M. doi:10.1073/pnas.86.3.953. PMC 286597. PMID 2915989.
- Prody CA, Zevin-Sonkin D, Gnatt A, Goldberg O, Soreq H (June 1987). "Isolation and characterization of full-length cDNA clones coding for cholinesterase from fetal human tissues". Proceedings of the National Academy of Sciences of the United States of America. 84 (11): 3555–3559. Bibcode:1987PNAS...84.3555P. doi:10.1073/pnas.84.11.3555. PMC 304913. PMID 3035536.
- Lockridge O, Adkins S, La Du BN (September 1987). "Location of disulfide bonds within the sequence of human serum cholinesterase". The Journal of Biological Chemistry. 262 (27): 12945–12952. doi:10.1016/S0021-9258(18)45149-6. PMID 3115973.
- McTiernan C, Adkins S, Chatonnet A, Vaughan TA, Bartels CF, Kott M, et al. (October 1987). "Brain cDNA clone for human cholinesterase". Proceedings of the National Academy of Sciences of the United States of America. 84 (19): 6682–6686. Bibcode:1987PNAS...84.6682M. doi:10.1073/pnas.84.19.6682. PMC 299147. PMID 3477799.
- Lockridge O, Bartels CF, Vaughan TA, Wong CK, Norton SE, Johnson LL (January 1987). "Complete amino acid sequence of human serum cholinesterase". The Journal of Biological Chemistry. 262 (2): 549–557. doi:10.1016/S0021-9258(19)75818-9. PMID 3542989.
- Jbilo O, Toutant JP, Vatsis KP, Chatonnet A, Lockridge O (August 1994). "Promoter and transcription start site of human and rabbit butyrylcholinesterase genes". The Journal of Biological Chemistry. 269 (33): 20829–20837. doi:10.1016/S0021-9258(17)31897-5. PMID 8063698.
- Mattes C, Bradley R, Slaughter E, Browne S (1996). "Cocaine and butyrylcholinesterase (BChE): determination of enzymatic parameters". Life Sciences. 58 (13): PL257–PL261. doi:10.1016/0024-3205(96)00065-3. PMID 8622553.
- Iida S, Kinoshita M, Fujii H, Moriyama Y, Nakamura Y, Yura N, Moriwaki K (1996). "Mutations of human butyrylcholinesterase gene in a family with hypocholinesterasemia". Human Mutation. 6 (4): 349–351. doi:10.1002/humu.1380060411. PMID 8680411. S2CID 86734543.
- Kamendulis LM, Brzezinski MR, Pindel EV, Bosron WF, Dean RA (November 1996). "Metabolism of cocaine and heroin is catalyzed by the same human liver carboxylesterases". The Journal of Pharmacology and Experimental Therapeutics. 279 (2): 713–717. PMID 8930175.
- Hidaka K, Iuchi I, Tomita M, Watanabe Y, Minatogawa Y, Iwasaki K, et al. (November 1997). "Genetic analysis of a Japanese patient with butyrylcholinesterase deficiency". Annals of Human Genetics. 61 (Pt 6): 491–496. doi:10.1046/j.1469-1809.1997.6160491.x. PMID 9543549. S2CID 23291616.
- Browne SP, Slaughter EA, Couch RA, Rudnic EM, McLean AM (July 1998). "The influence of plasma butyrylcholinesterase concentration on the in vitro hydrolysis of cocaine in human plasma". Biopharmaceutics & Drug Disposition. 19 (5): 309–314. doi:10.1002/(SICI)1099-081X(199807)19:5<309::AID-BDD108>3.0.CO;2-9. PMID 9673783. S2CID 35577799.
- Altamirano CV, Lockridge O (October 1999). "Conserved aromatic residues of the C-terminus of human butyrylcholinesterase mediate the association of tetramers". Biochemistry. 38 (40): 13414–13422. doi:10.1021/bi991475+. PMID 10529218.
- Darvesh S, Kumar R, Roberts S, Walsh R, Martin E (June 2001). "Butyrylcholinesterase-Mediated enhancement of the enzymatic activity of trypsin". Cellular and Molecular Neurobiology. 21 (3): 285–296. doi:10.1023/A:1010947205224. PMID 11569538. S2CID 9861675.
- Barta C, Sasvari-Szekely M, Devai A, Kovacs E, Staub M, Enyedi P (December 2001). "Analysis of mutations in the plasma cholinesterase gene of patients with a history of prolonged neuromuscular block during anesthesia". Molecular Genetics and Metabolism. 74 (4): 484–488. doi:10.1006/mgme.2001.3251. PMID 11749053.
External links
[edit]- Butyrylcholinesterase at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Human BCHE genome location and BCHE gene details page in the UCSC Genome Browser.